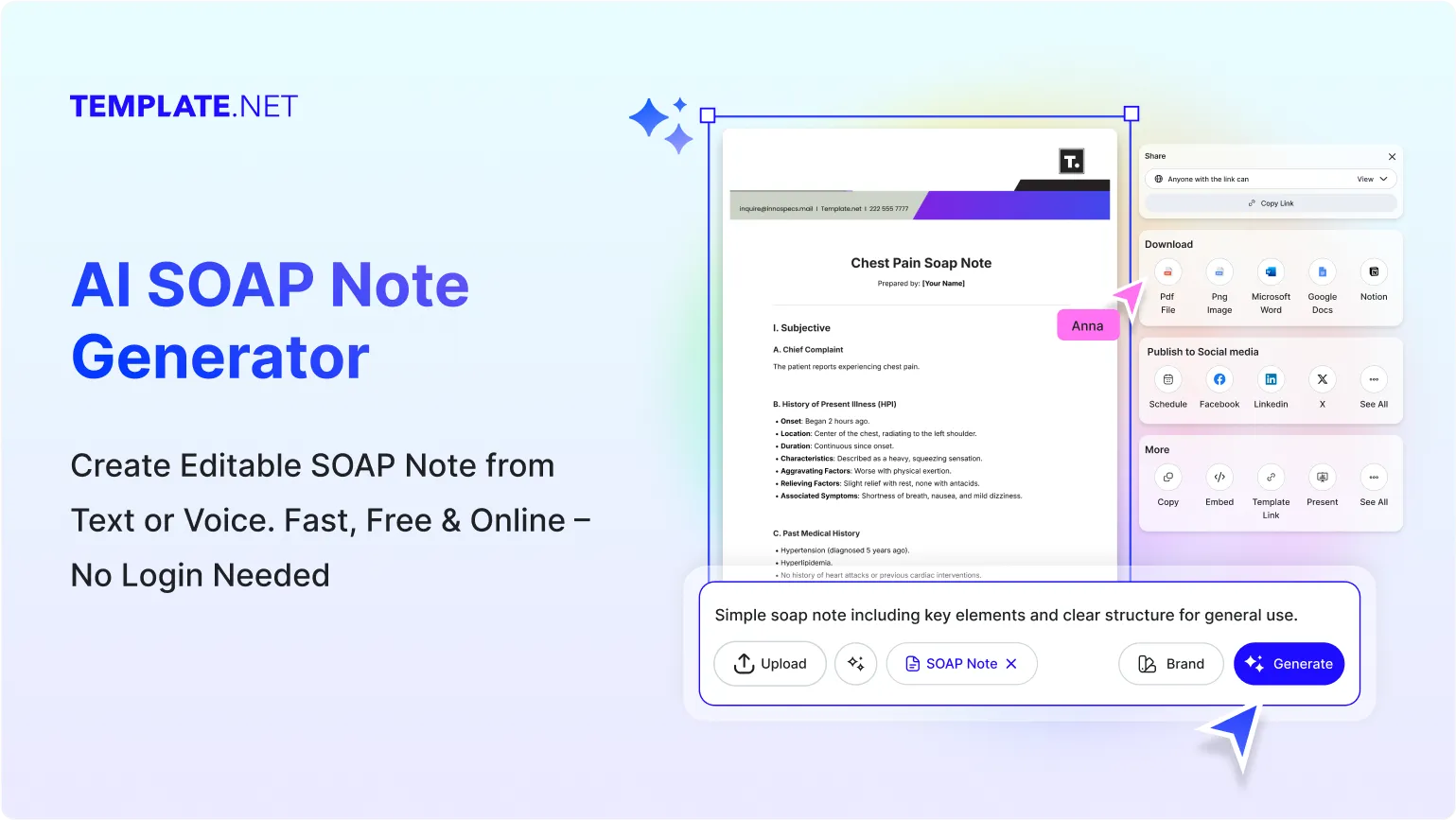
Free AI SOAP Note Generator
Create SOAP Notes, Edit online with AI-Powered SOAP Note Editor
Template.net’s Free AI SOAP Note Generator helps you draft high-quality SOAP notes in seconds. Edit online with your brand logo, fonts, tone, and custom elements to ensure every SOAP note is personalized and professional. Whether you're documenting patient updates, therapy sessions, or clinical assessments, stay on-brand and on-point. Download in multiple formats, share instantly, and communicate with clarity and confidence.
Write Custom, Professional SOAP Notes in Seconds
From therapy notes to medical assessments, our AI-powered document writer helps you craft polished, on-brand content in any format, tone, or language. No blank pages, no formatting guesswork.
AI Brand Voice
Choose from formal, conversational, passive, or empathetic note styles. Our AI rewrites your SOAP note to match your message whether you’re documenting clinical updates or patient history. You can also generate content in your brand’s voice, complete with tone, style, and branded notes for total consistency.
AI-Smart Formatting Suggestions
Get instant suggestions for improving structure, layout, headings, and flow especially useful for structured SOAP note documentation.
Multiple Document Types Supported
Generate a wide range of SOAP note formats including initial assessments, progress notes, discharge notes, therapy updates, treatment plans, and follow-up reviews.
Clinical & Professional Formatting
Support for SOAP-aligned medical formatting and terminology. Ideal for hospitals, outpatient settings, rehabilitation centers, and academic medical institutions.
Smart Personalization
Auto-fill patient names, dates, conditions, session types, and other context-aware details to save time and reduce repetitive writing.
Auto-Suggested Visuals & Headers
Let AI recommend headings like Subjective, Objective, Assessment, Plan and related subsections to ensure clean, structured documentation.
Multilingual Note Generation
Generate notes in 20+ global languages using text or voice prompts.
Languages supported: English, Spanish, French, Hindi, Arabic, Chinese, Portuguese, Bengali, Russian, Japanese, German, Korean, Italian, Turkish, Vietnamese, Urdu, Persian, Polish, Thai, and Punjabi. Perfect for multilingual hospitals or global teams.
Voice-Powered Drafting
On the go? Just speak your prompt and let the AI generate your SOAP note hands-free and instantly.
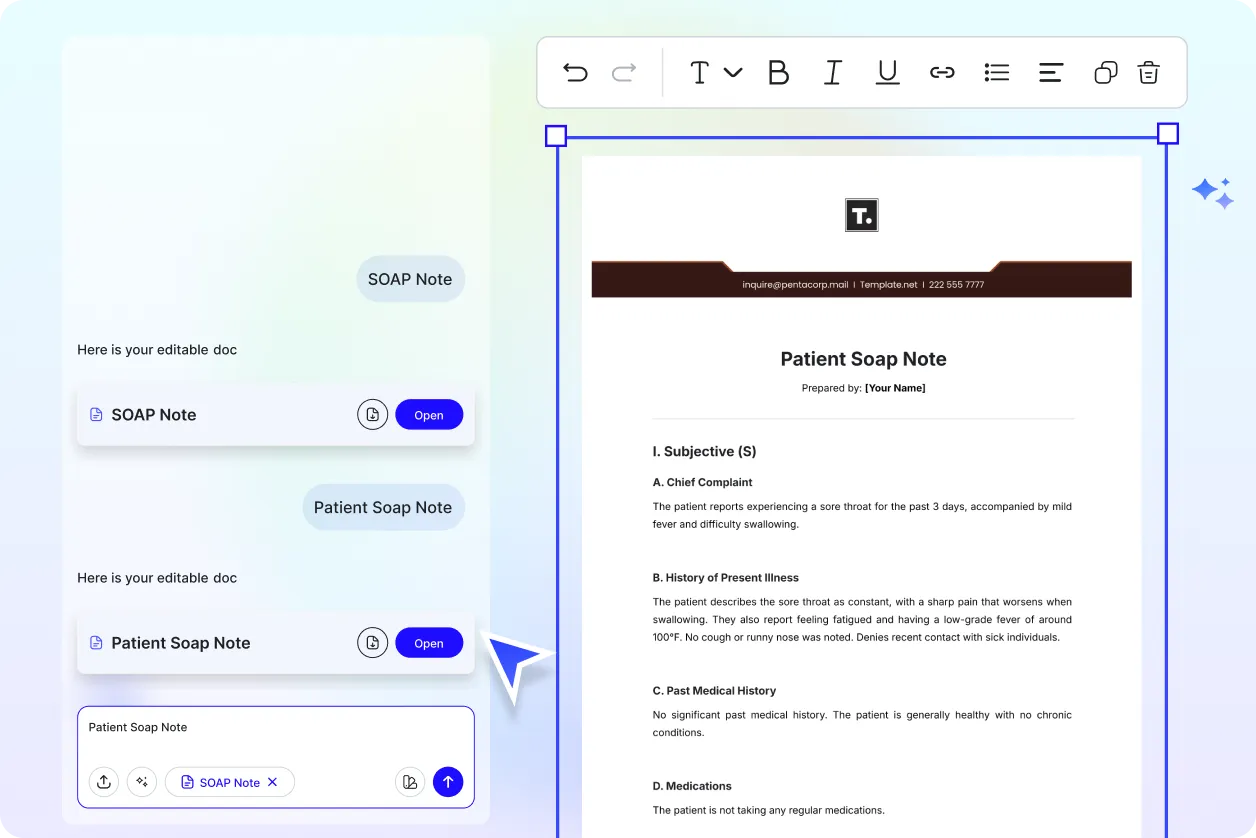
Fully Customizable Text, Styles and Design
Easily update fonts, headings, colors, and layout. Apply branding using built-in design controls with support for customizable headers and templates
Branding and Visual Control
Apply your logo, font style, and colors automatically to maintain consistency across all clinical notes.
Real-Time Proofreading
Check for medical grammar, punctuation, and terminology in real-time without needing external tools.
Rewriting and Content Expansion
Ask AI to rephrase, summarize, or expand any SOAP note section based on tone and content.
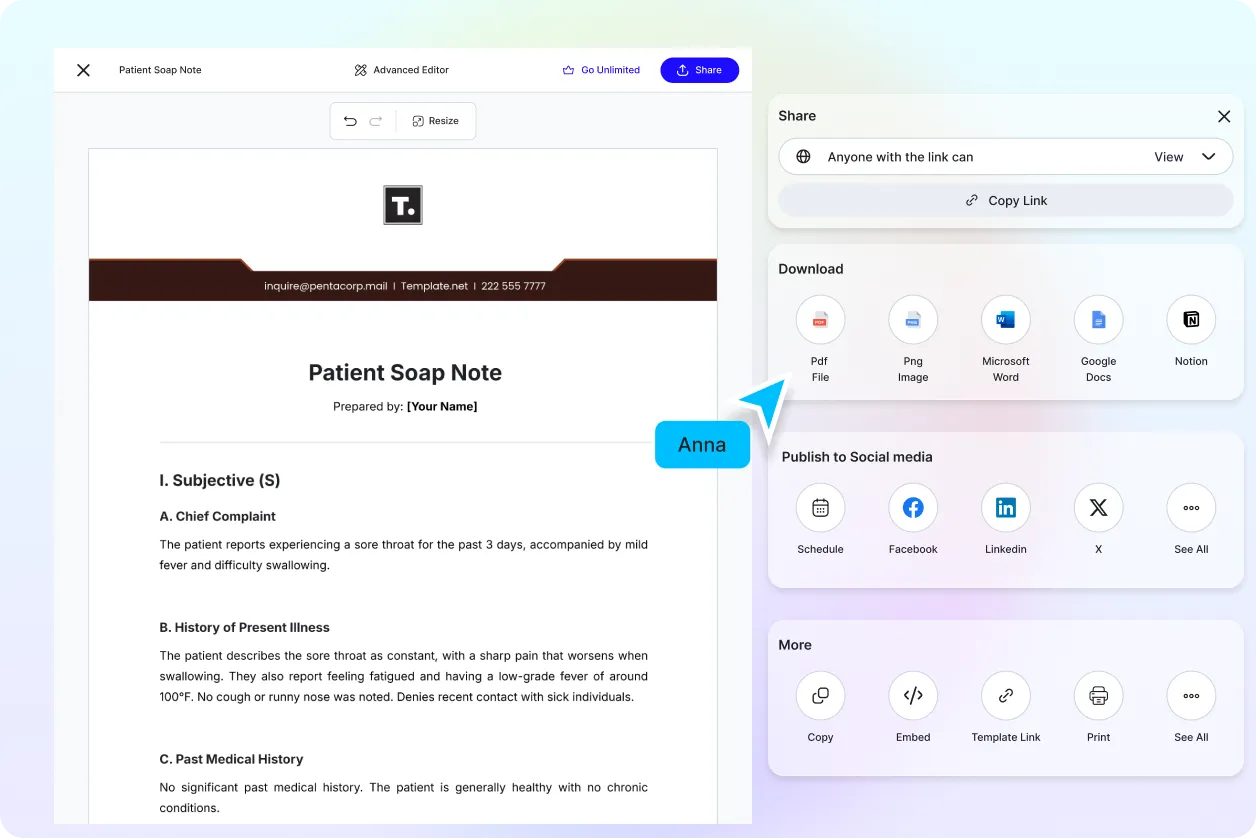
Export in Multiple Formats
Download documents in DOCX, PDF, TXT, PNG, or HTML formats. Supports export to cloud services or clinical systems.
Real-Time Collaboration
Work live with peers or supervisors. Add comments, edit notes, and finalize documentation together in one shared workspace.
Translate Full Documents Instantly
Translate SOAP notes and other documents with one click ideal for multilingual patients or global medical teams.
Share or Embed Anywhere
Publish using link, QR code, or embed option to include notes in portals, platforms, or knowledge bases.
Secure Cloud Workspace
Store SOAP notes securely, assign roles, and control access for clinical teams with full data protection.
Add Signature Blocks
Insert digital signature fields for clinician approvals or formal sign-offs in SOAP documentation.
Attach Files and Media
Embed reports, lab results, audio files, or supporting media directly inside your SOAP note.
Add Images and Videos
Insert diagrams, scans, or instructional visuals to enhance clarity and engagement.
Add Tables and Structured Data
Insert responsive tables to organize medications, vitals, care timelines, or therapy comparisons.
AI-Linked Plan Recommendations
Based on the Assessment section, the AI intelligently suggests treatment plans, follow-up actions, or referrals that align with clinical best practices.
SOAP Section Autofill
Automatically generate each SOAP section based on your input to save time and maintain consistent formatting
Clinical Terminology Suggestions
AI suggests medically accurate terms while writing SOAP notes to ensure clarity and professionalism.
How to Write a Free AI-Generated SOAP Note
Just enter a prompt, customize the draft, and export your polished SOAP note in minutes. No formatting, no friction.
Step 1: Start with a Prompt
Type or speak your SOAP note’s purpose such as "Patient follow-up for knee pain", "Initial mental health evaluation", or "Therapy progress update". Our AI instantly understands your intent and starts drafting.
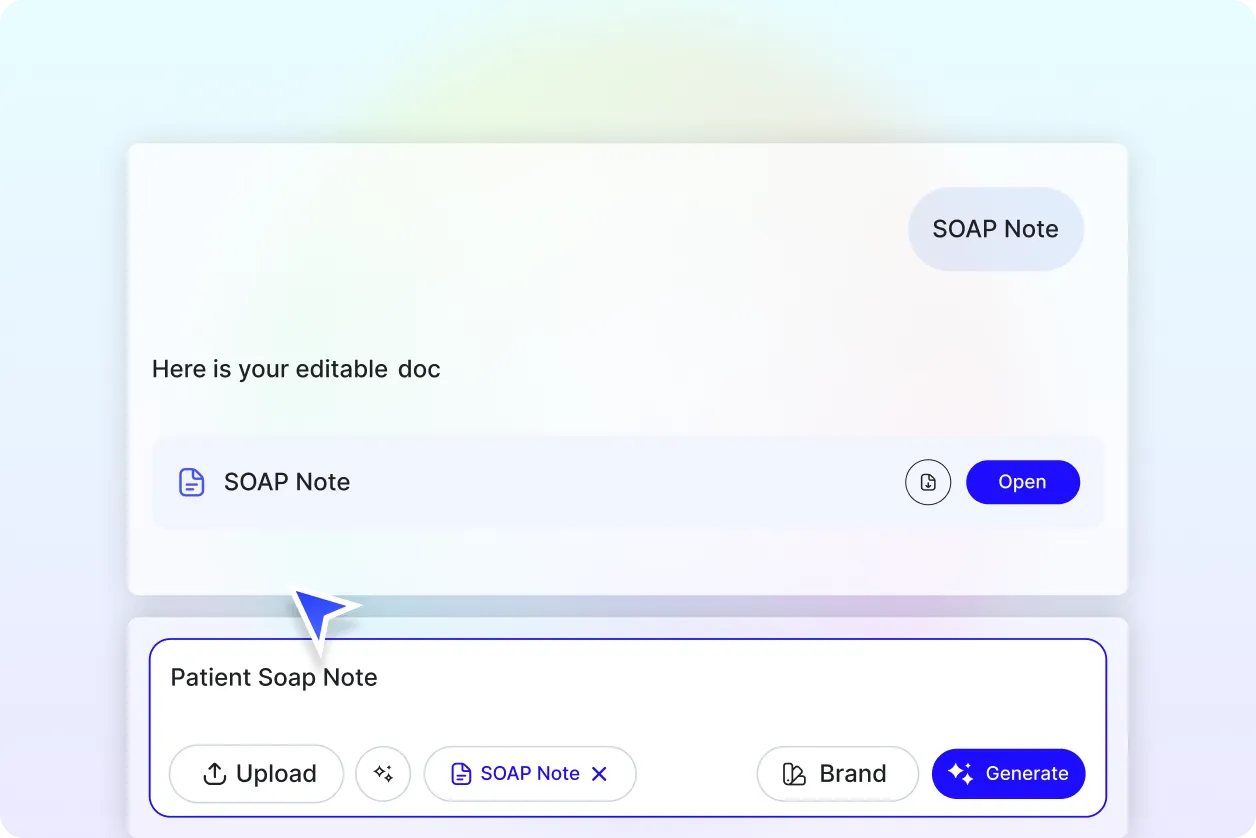
Step 2: Generate and Edit
Within seconds, you’ll see a professionally written SOAP note tailored to your prompt. Refine the tone, structure, or content or regenerate multiple versions to explore different directions.
Step 3: Finalize and Share
Add patient details, your name, or any clinical formatting. Then export your note in DOCX, PDF, TXT or share it instantly via Email, LinkedIn, WhatsApp, Facebook, X (Twitter), Pinterest, Reddit or generate a live link or QR code for seamless delivery.
Work Smarter and Promote Your Brand
Generate SOAP Notes That Represent You
Apply your clinic’s brand style in seconds. From section headers to voice, every element of your SOAP note reflects your identity.
Reuse, Repeat, and Scale Easily
Save high-performing SOAP notes as reusable templates. Adjust details and resend across patient visits or departments without rewriting from scratch.
Share Instantly, Collaborate Smoothly
Download or export SOAP notes in DOCX, PDF, TXT. Share online, collaborate live, and receive feedback without scattered emails or files.
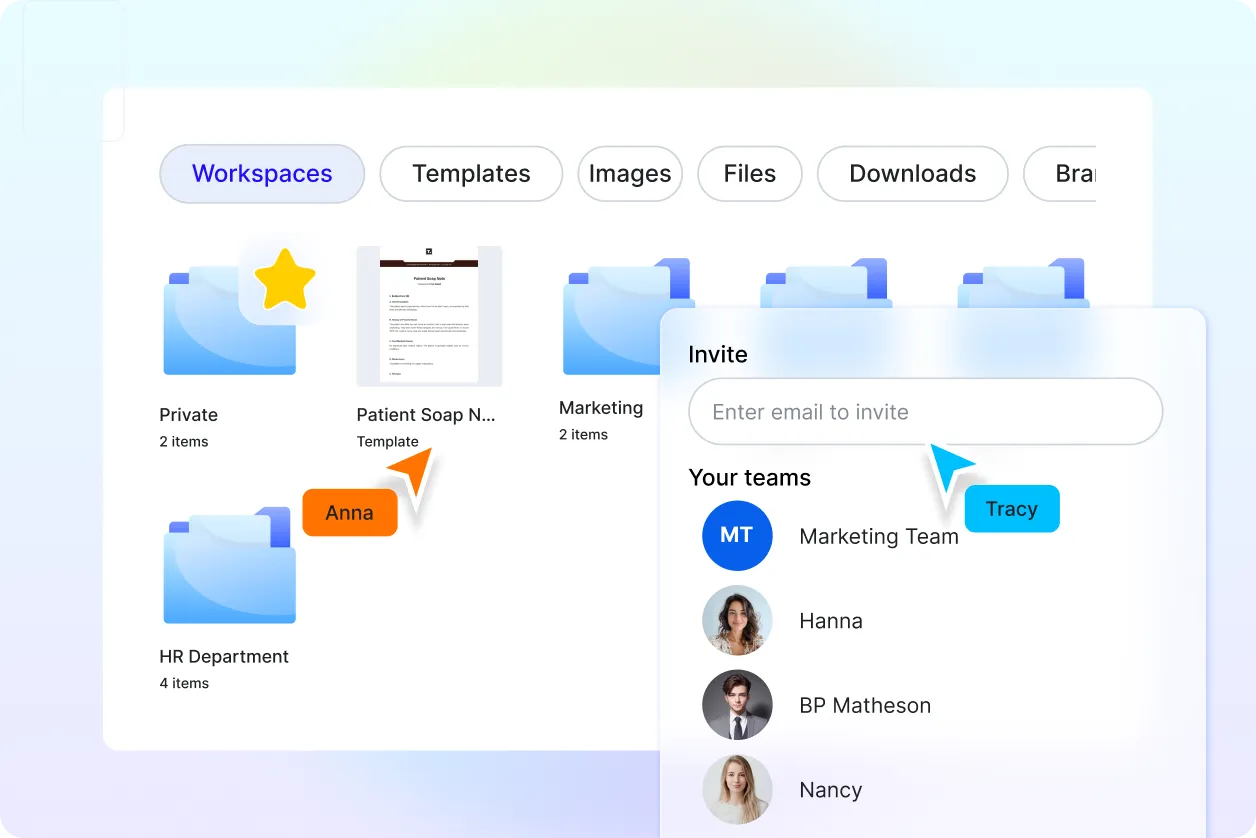
Smart Workspaces for Teams
Create centralized hubs for SOAP note projects. Assign access levels, store brand elements, and keep every session aligned across teams.
SOAP Note FAQ
What is a SOAP note and how is it used?
A SOAP note is a structured format used by healthcare professionals to record patient information including symptoms, observations, evaluations, and treatment plans. It helps document progress clearly and professionally.
How do I write a SOAP note using AI?
Simply enter a short prompt like "back pain evaluation for follow-up visit" or speak using voice input. The AI will instantly generate a structured SOAP note with Subjective, Objective, Assessment, and Plan sections in a clear and professional format.
Can I generate SOAP notes in different languages or regions?
Yes. You can create clinically formatted SOAP notes in over 20 global languages using text or voice input.
Languages supported: English, Spanish, French, Hindi, Arabic, Chinese, Portuguese, Bengali, Russian, Japanese, German, Korean, Italian, Turkish, Vietnamese, Urdu, Persian, Polish, Thai, and Punjabi. The AI adjusts formatting for local and international standards where needed.
How can I export or share my SOAP note?
You can export the note in DOCX, PDF, or TXT, or copy it directly into clinical systems or workspaces. Share through email, public link, or QR code, or post to platforms such as LinkedIn, WhatsApp, Facebook, Twitter, and more.
How do I format a SOAP note correctly?
A proper SOAP note includes a clear Subjective section, Objective details, an Assessment summary, and a Plan of action. The AI applies proper spacing and headers to ensure consistent clinical documentation.
Can I rewrite or improve an existing SOAP note with AI?
Yes. Just paste your draft, and the AI can restructure it or improve tone and clarity while keeping your original message and medical content intact.
Can I add signatures, visuals, or other elements to my SOAP note?
Absolutely. You can insert signature blocks, attach files like lab reports, or add diagrams and branding elements if required. This is useful for formal documentation and internal reviews.