Best AI Text to Video Models & Templates
1. Google Gemini / Veo 3.1 https://images.template.net/wp-content/uploads/2025/12/Google-Gemini-Veo-3.1.mp4 This Google Gemini tool is for creating high-quality AI videos from text or…
Mar 21, 2024
Most sick patients long for a hospital discharge because the event signifies an improvement in their health. But do you ever wonder how physicians (and the entire nursing care team) ensure that all the medical care given to a patient is recorded and made available for their next outpatient visit? It is simple—the healthcare industry uses discharge summary templates.
If you are looking for samples of discharge summary templates in word, you have come to the right corner of the Internet. In this article, we will provide tips for creating these free templates for your own organization through different downloadable discharge summary samples. We have also included a few health-teaching techniques that the healthcare team may implement to ensure post-hospital discharge patient compliance.
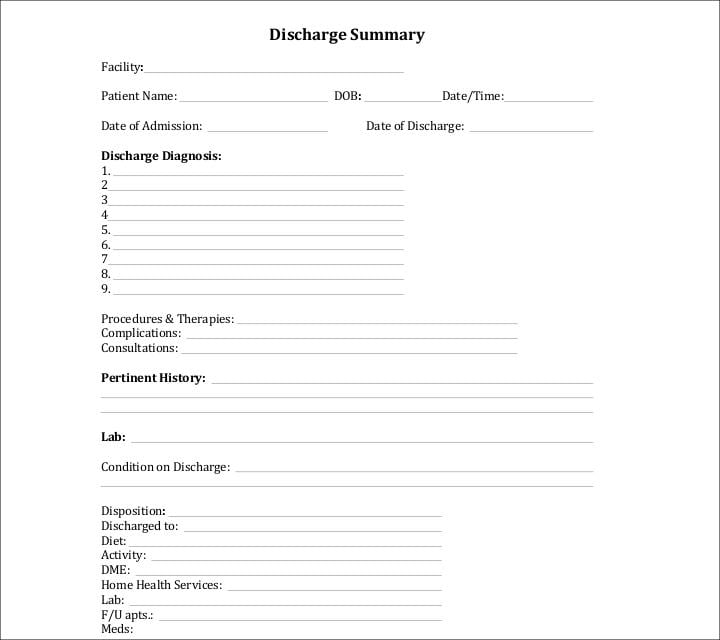
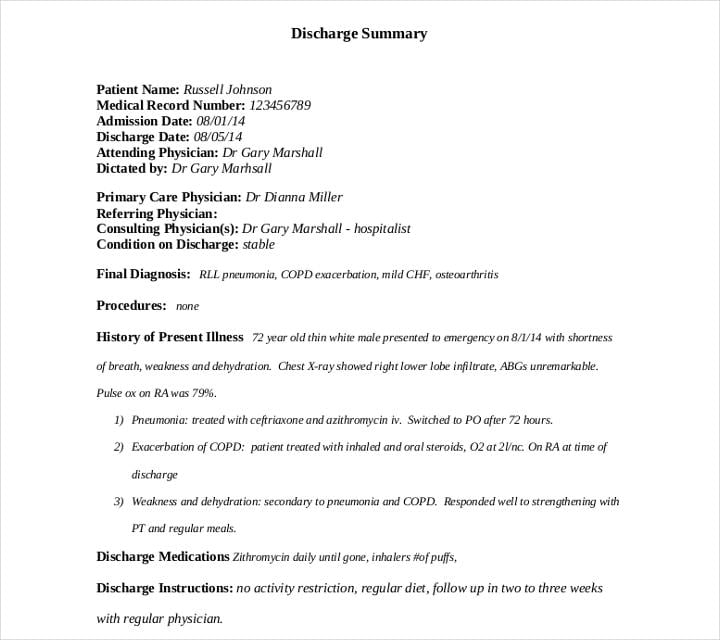
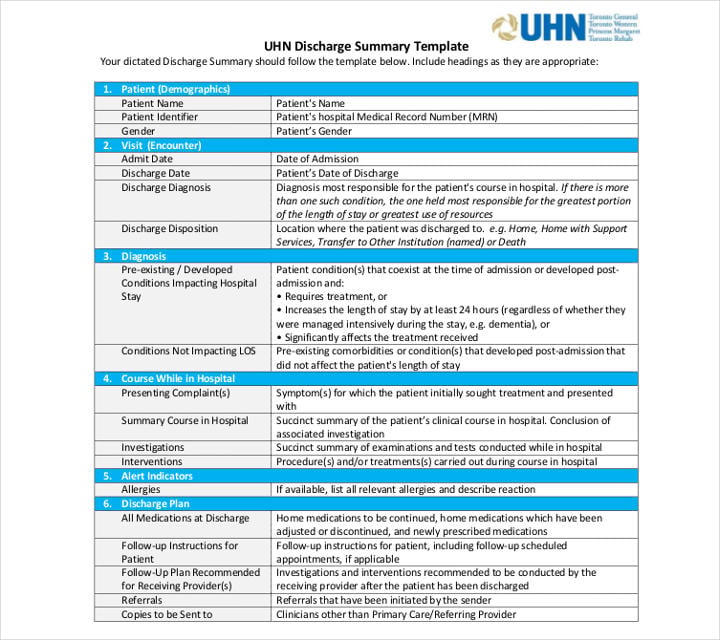
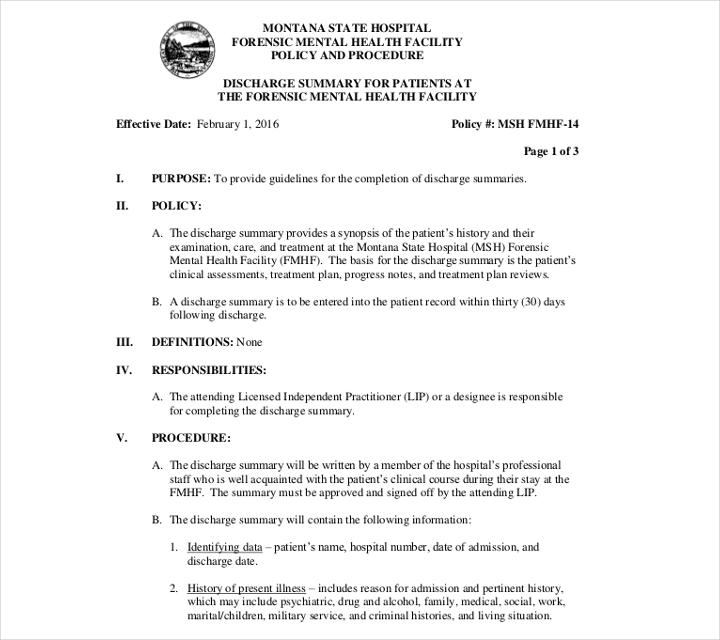
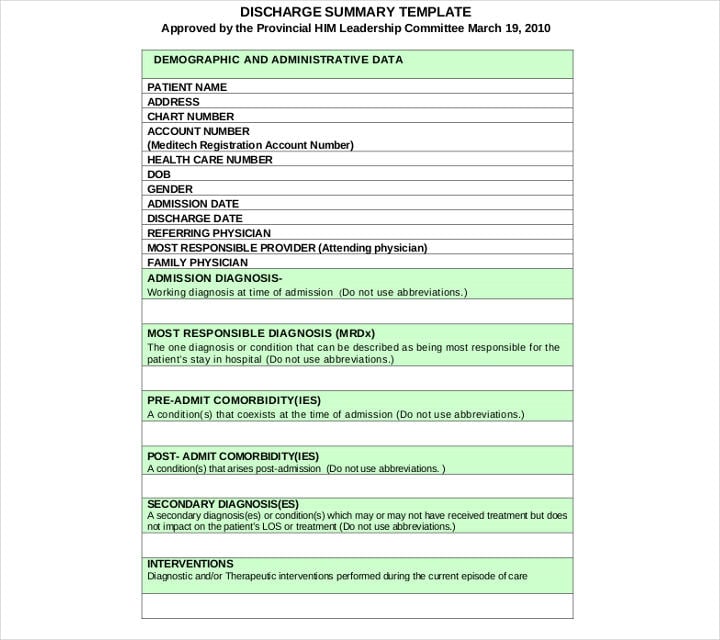
In essence, discharge summary templates are documents (usually printed) that contain all the health information pertaining to the patient’s stay at a hospital or healthcare facility. As a summary template, all information is written in brief and concise points. It will also include an intended care plan for the patient after he or she is discharged from the facility. All discharge summary templates and forms are treated as confidential since they are part of the patient’s personal health information and may not be accessed without authorization from the patient, his or her legal representative, or the court.
Most hospitals and clinics have their own formats for their discharge summary templates. Some states and governments may also require public and state-funded health facilities to use a certain discharge form. However, the respective hospitals will have the final say in the specific design template they want to use for the discharge form.
We will primarily focus on discharge summary templates created and used by organizations in the healthcare industry like hospitals, clinics, mental health facilities, and teaching universities. Note that there can be other types of discharge summary templates used in other industries. For example, a discharge summary may also be used in military and para-military organizations. Additionally, note that a discharge summary template is different from a medical report template.
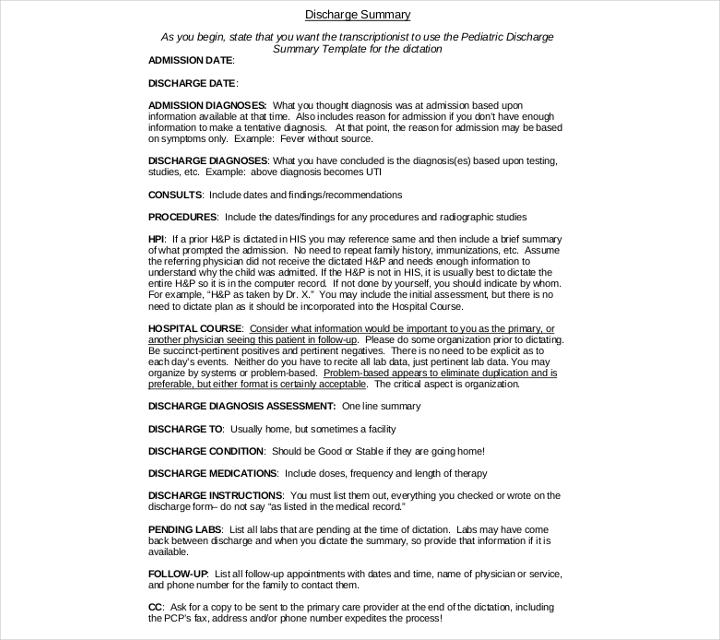
In some countries, all healthcare facilities are required to fill out a standardized discharge summary template for all their patients. In the United States, there is no single discharge summary form created but most healthcare institutions follow the same guidelines in their discharge summary templates. Listed below are the most important items that should be included in a discharge summary.
caltcm.org
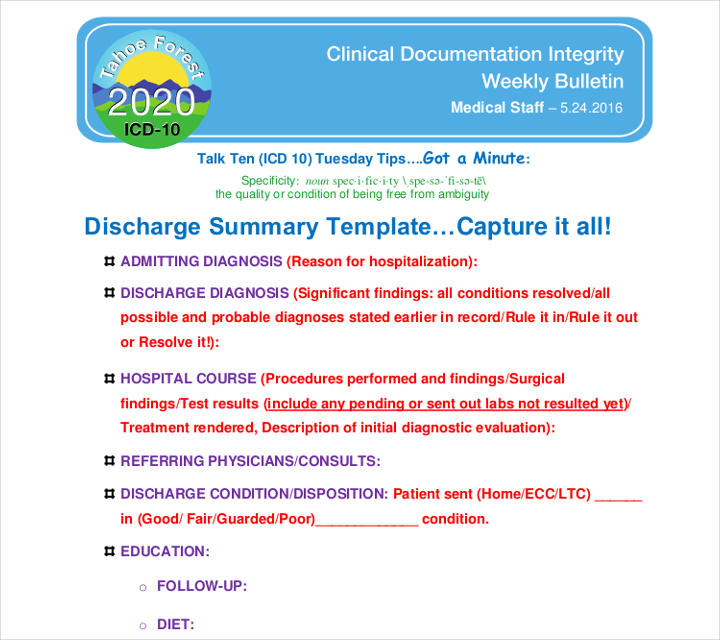
tfhd.com
A discharge summary is a kind of document which has all the necessary details about the health condition of a patient and their time in a hospital. All the information are written concisely. Any forms of ambiguity are avoided for understanding. If you are looking for creating a discharge summary in google docs, make sure you include the following points. Sometimes, every physician gives a different discharge summary. It should consist of the following points:
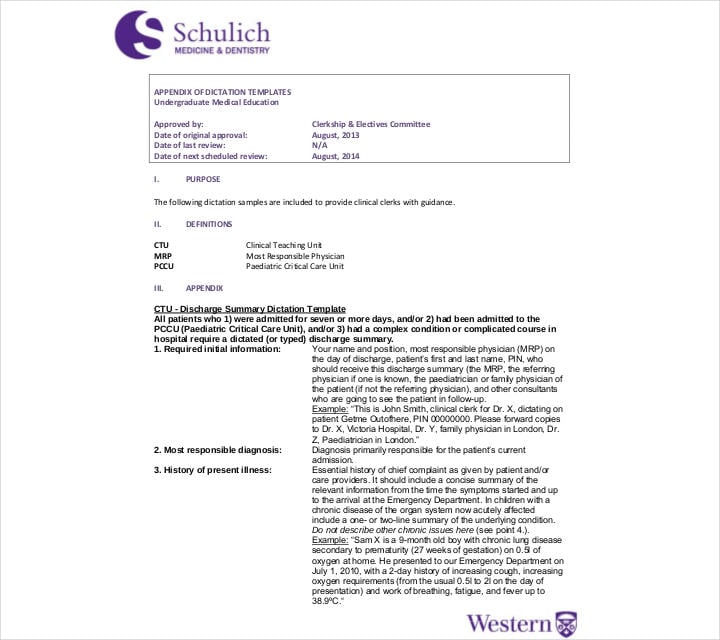
schulich.uwo.ca
idph.iowa.gov
uhnmodules.ca
Physicians are required to write discharge summaries for all their patients whether they recover from their illnesses or not. Aside from being a mandatory sample policy, we have listed below the numerous other uses of discharge summaries that every member of the healthcare team should know.
hiqa.ie
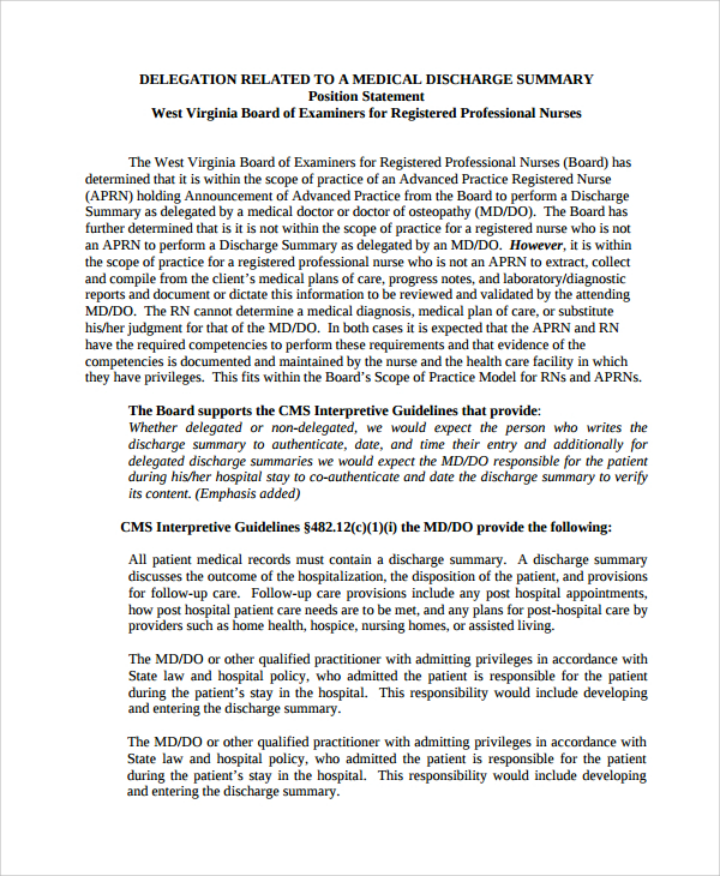
wvrnboard.wv.gov
residency.pediatrics.med.ufl.edu
dphhs.mt.gov
nlchi.nl.ca
One of the main benefits of creating discharge summaries is that it allows the physician (and the entire healthcare team) to create a holistic treatment plan for the patient even after their contact with the patient ends. This is primarily done by providing the patient (and his/her significant other) with applicable health teachings. When done right and with the patient’s cooperation, you can almost always guarantee fast recovery and decrease the risk of recurrence of the illness.
We hope you were able to learn more about hospital discharge forms from this article. Do check out the other posts on our website for information on a variety of topics.
1. Google Gemini / Veo 3.1 https://images.template.net/wp-content/uploads/2025/12/Google-Gemini-Veo-3.1.mp4 This Google Gemini tool is for creating high-quality AI videos from text or…

In today’s fast-paced digital world, efficiency and consistency are key to content creation, and this is where the power of…
Hospitality Induction Templates are structured guides created specifically for the hospitality industry to facilitate the onboarding process for new employees.…
Whether you are a business or an organization, it is important for you to keep track of your business bank…
A Company Description provides meaningful and useful information about itself. The high-level review covers various elements of your small business…

A smartly designed restaurant menu can be a massive leverage to any food business.
Whether you need to keep neat records of received payments, or are looking for a template that helps you look…
The most widely recognized use for a sample letter of planning is the understudy who, after finishing secondary school, wishes…
The term “quotation” can refer to several things. While to some it may refer to a quote, which is proverbial.…