11+ Logistics Note Templates in PDF | MS Word
Taking down notes is a common practice on businesses, and it becomes familiar for every worker since note-taking happens even…
Sep 21, 2023
SOAP (subjective cues, objective cues, assessment, and planning) is a tool that most health care providers use when dealing with patients. It involves taking the patient’s verbal cues regarding his/her condition and getting their vital signs (temperature, heart rate, breathing rate, blood pressure), making an assessment based on their condition, and a plan of care. Based on this, the providers can then render the appropriate interventions to the patient, and after which, an evaluation will be made to determine whether or not there has been an improvement in the patient’s condition.

On our website, we provide you with note templates utilizing the SOAP format to be used by nurses, nursing students, doctors, dietitians, therapists, and any health care professional directly handling patients. The templates have been readily made, and a generous amount of space is provided for you to write the information you need gathered from the patients.
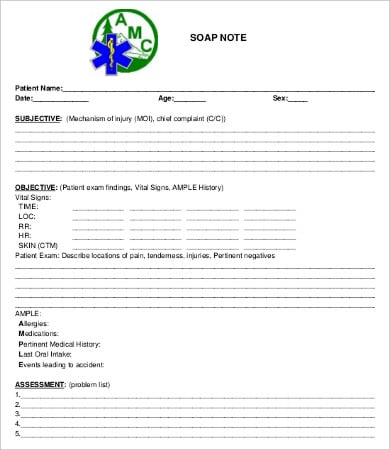 amcdv.org
amcdv.org expertsintherapy.com
expertsintherapy.com gwendolynchildress.weebly.com
gwendolynchildress.weebly.com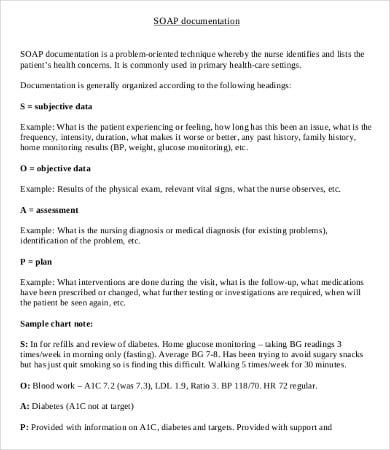 nurseone.ca
nurseone.ca higherdoc.info
higherdoc.infoHere are some reminders and a more detailed explanation we offer on how to effectively write your SOAP notes:
Through the use of SOAP, providers will have an idea on what the patient is feeling and can simple plan ahead on what to do for their patients’ condition. After which, providers can also then record the interventions performed on the patient and evaluate the effects of the said actions. Providers can then compare the expected outcome with the actual results.
Our website hosts an array of templates, specifically for nutritionists, for them to assess the nutritional status of the patient and make plans on the patient’s diet. We have templates for the medical staff to also give them a record on the progress of the patient during the time he/she was admitted
For physical therapists, to help them determine the muscular capabilities and the motor skill of the patient, we also have templates to be used specifically on pediatric patients and another one to be used on newborn patients. We have daily SOAP templates, and we also have a simplistic blank templates, which give the writer more freedom on what to write.
For simple templates about handling conflicts and issues, check out our collection of Briefing Note Templates.
 csun.edu
csun.edu unm.edu
unm.edu amtamassage.org
amtamassage.org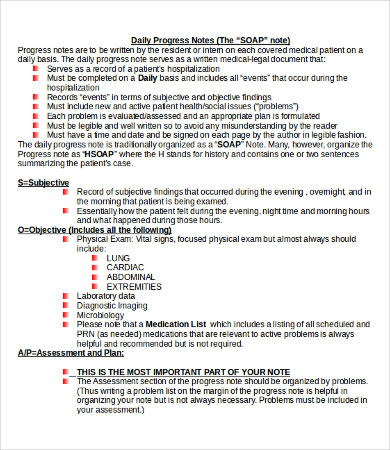 berkshirehealthsystems.org
berkshirehealthsystems.org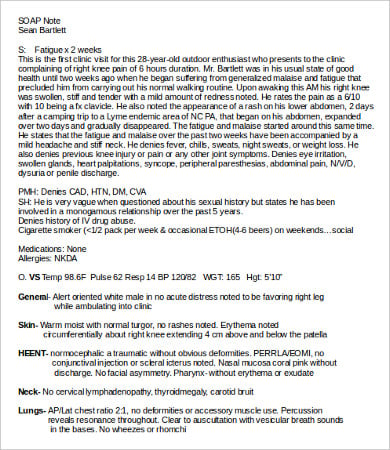 lhup.edu
lhup.eduThese SOAP notes templates have been made to suit any health care provider’s needs. They can easily be downloaded from our website, free of charge. They come in Doc, Docx, and high-resolution PDF formats and are fully editable. Simply download the template on your computer and print them on a regular coupon bond.
If you are looking for other sample templates, our website also has Credit Note Templates. For even more templates to choose from, scroll to the bottom and feel free to check out the links to other templates that we provide on our website.
Taking down notes is a common practice on businesses, and it becomes familiar for every worker since note-taking happens even…
A printable doctor’s note is a crucial document for employees needing to verify medical absences. It serves as official proof…
A doctor attends to many patients in a day thereby making it difficult to remember the case history of each…

A doctor’s note, or commonly referred to as a medical certificate or sick note, is a verification from a doctor…

An investment promissory note can be referred to as a legal document that compels the person who signs this form…
A credit note is a statement issued and sent to the purchaser by a vendor which certifies that a credit…

A register or a set of notes that is maintained by the audit staff to record some important points observed,…

An absent note is any formally framed letter that’s self-addressed to any senior or body member for not attaining the…

In the simplest of terms, a promissory note refers to a ‘promise to pay.’ In other words, it is a…