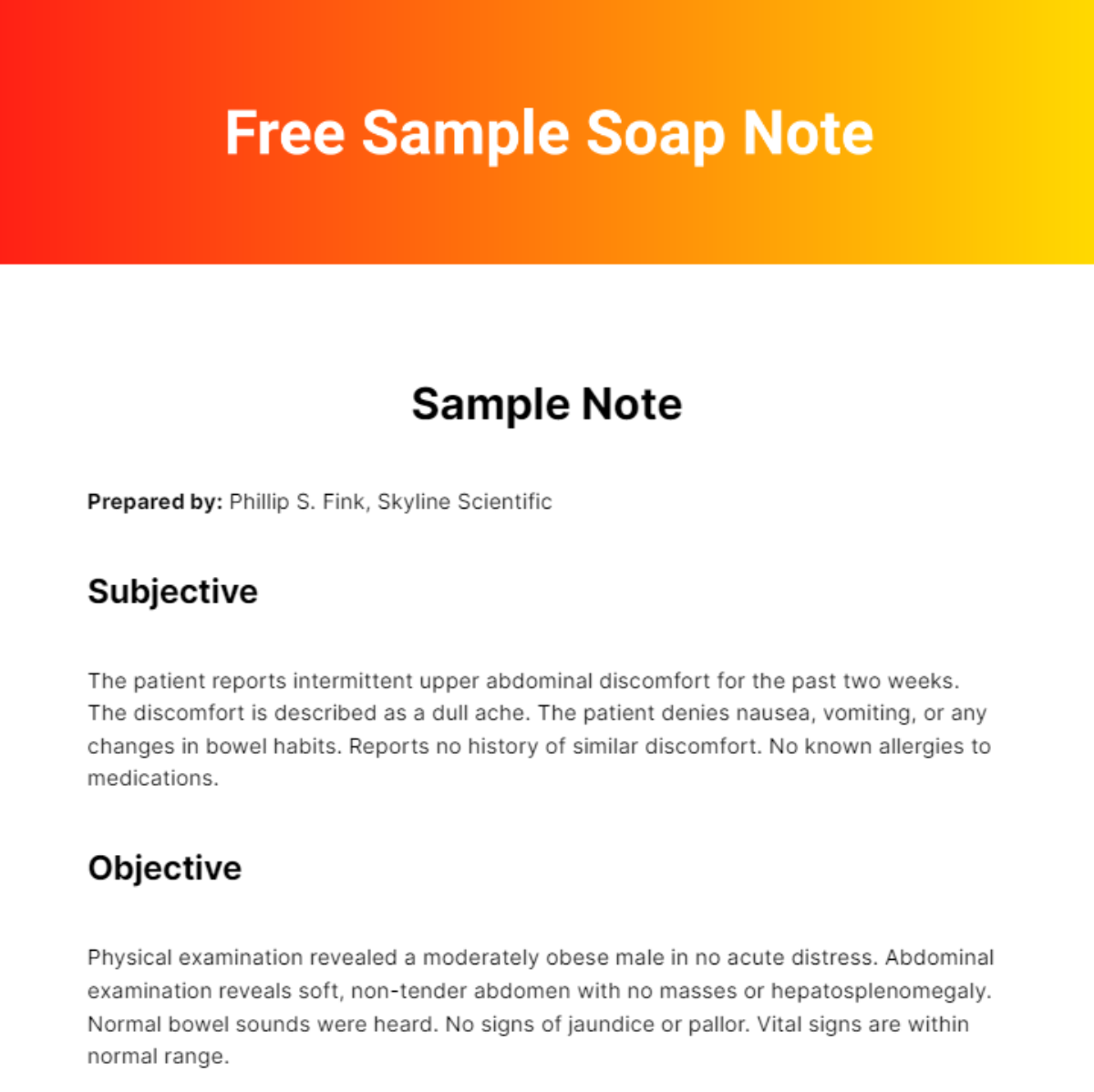
Sample Note
Prepared by: Phillip S. Fink, Skyline Scientific
Subjective
The patient reports intermittent upper abdominal discomfort for the past two weeks. The discomfort is described as a dull ache. The patient denies nausea, vomiting, or any changes in bowel habits. Reports no history of similar discomfort. No known allergies to medications.
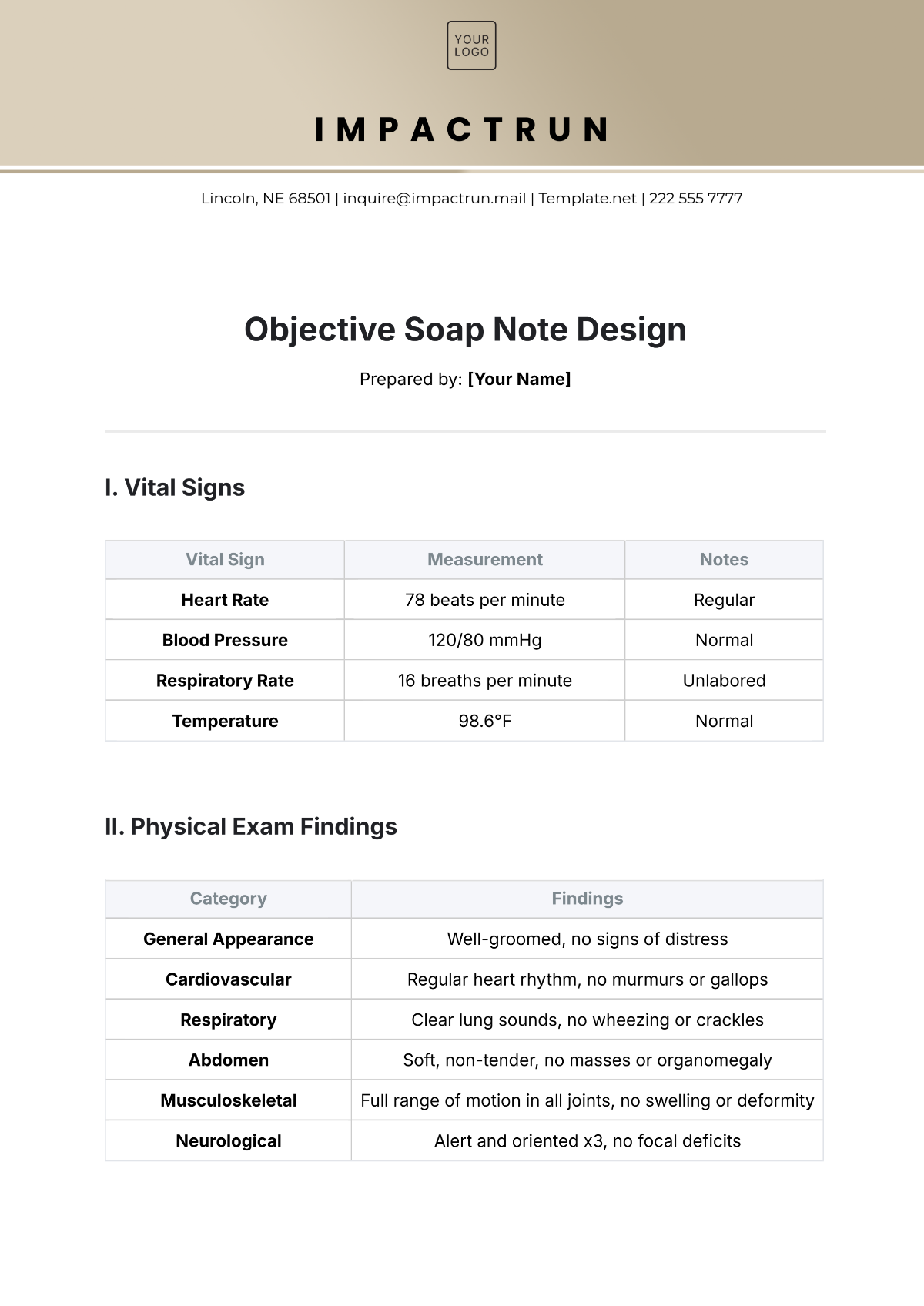
Objective
Physical examination revealed a moderately obese male in no acute distress. Abdominal examination reveals soft, non-tender abdomen with no masses or hepatosplenomegaly. Normal bowel sounds were heard. No signs of jaundice or pallor. Vital signs are within normal range.
Assessment
The intermittent upper abdominal discomfort could suggest possible gastritis or gallstones, though symptoms are not severe or consistent enough to suggest acute cholecystitis or peptic ulcer disease. Further diagnostic evaluation may be necessary if symptoms persist.
Plan
We have recommended lifestyle modifications for Gastritis including avoidance of triggers such as spicy food, alcohol, and stress. Over the counter antacids can also be utilized for symptom relief. For potential gallstones, we have advised a watchful waiting approach as the symptoms are currently not severe. A follow-up appointment in two weeks, or sooner if symptoms worsen.
Prepared by: Phillip S. Fink
Skyline Scientific
Telephone: 222 555 7777
Email: PhillipSFink@gmail.com
Address: 320 Skyward Road, Boulder, CO 80302, USA
Company Email: SkylineScientific@gmail.com