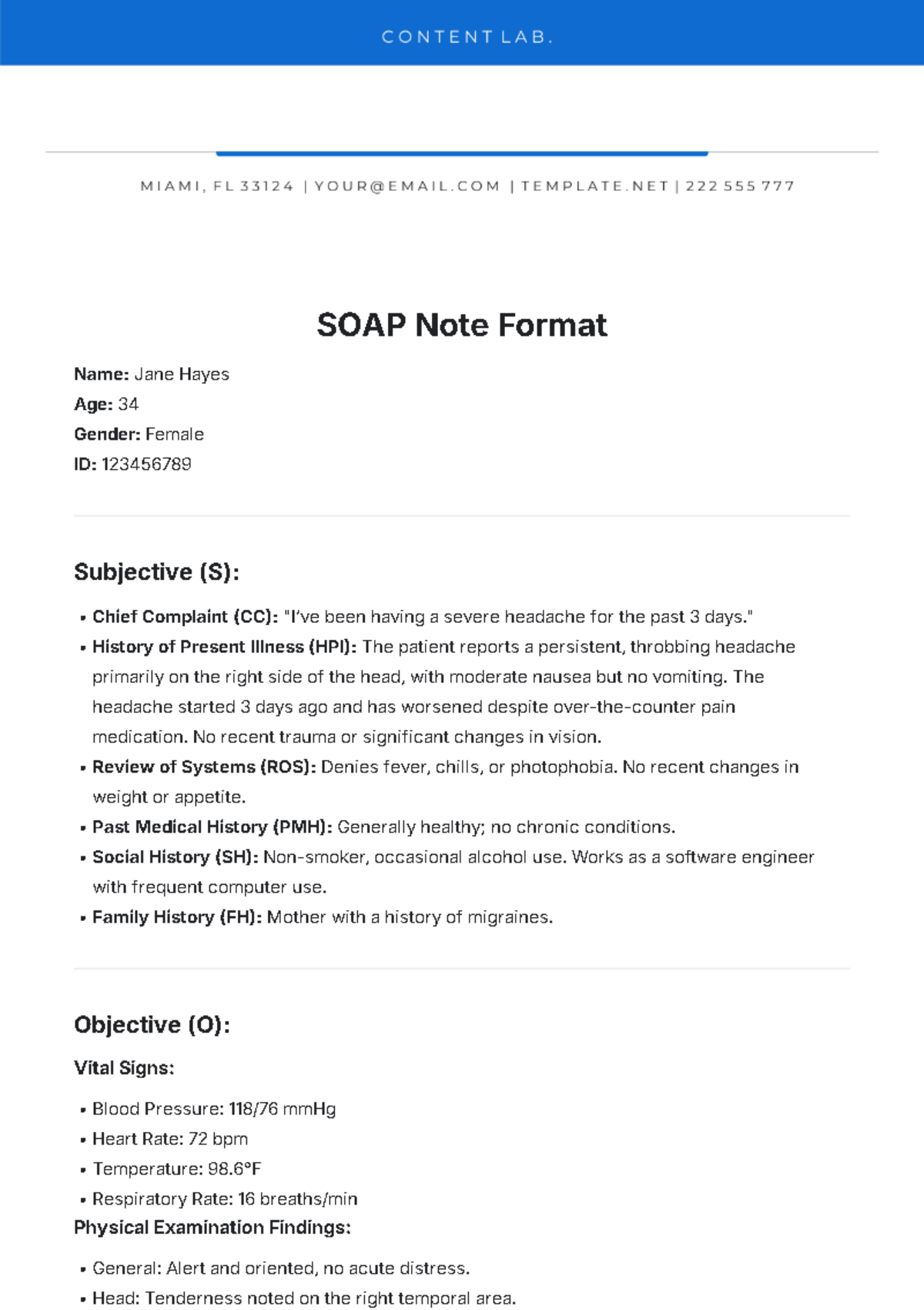
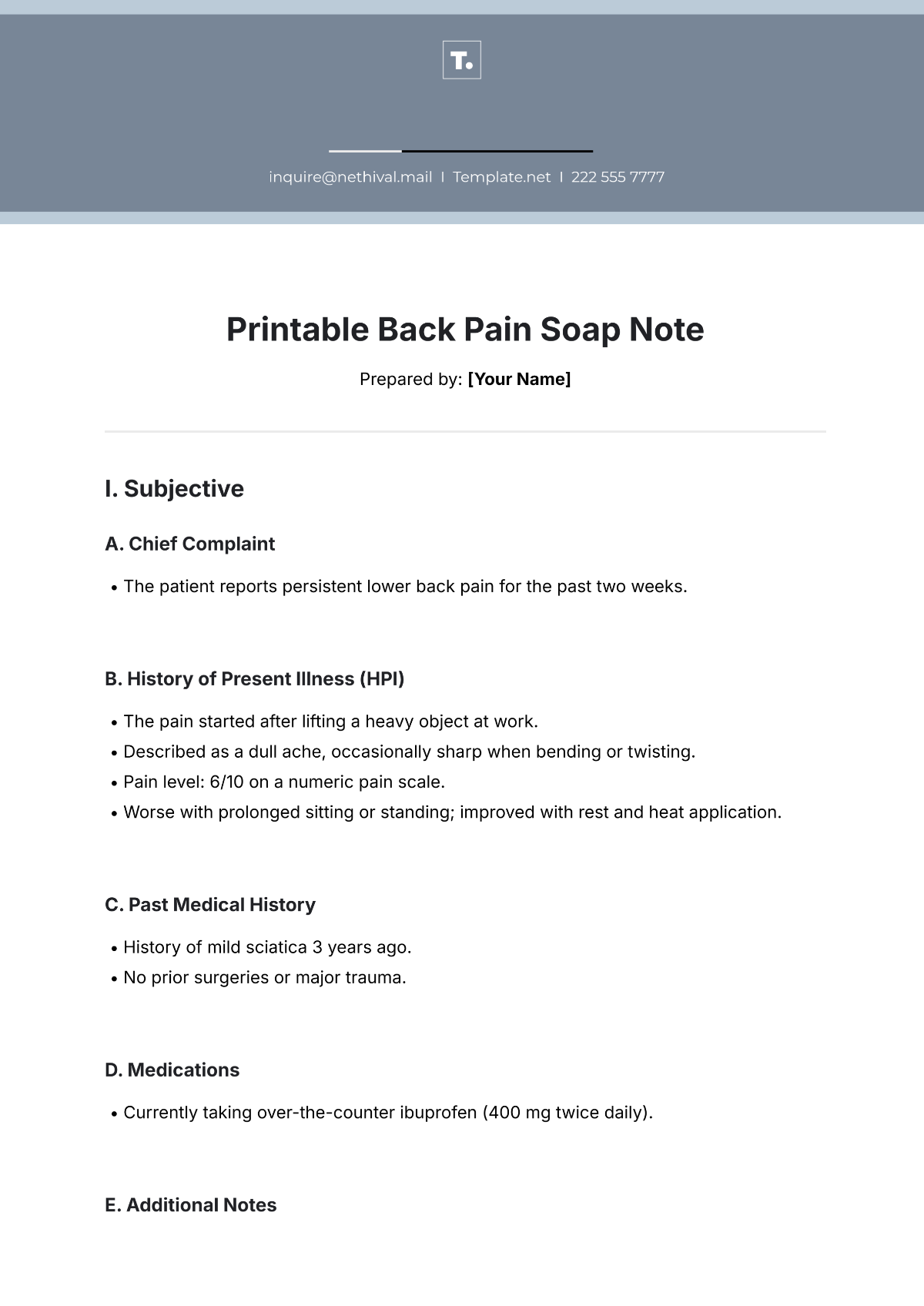
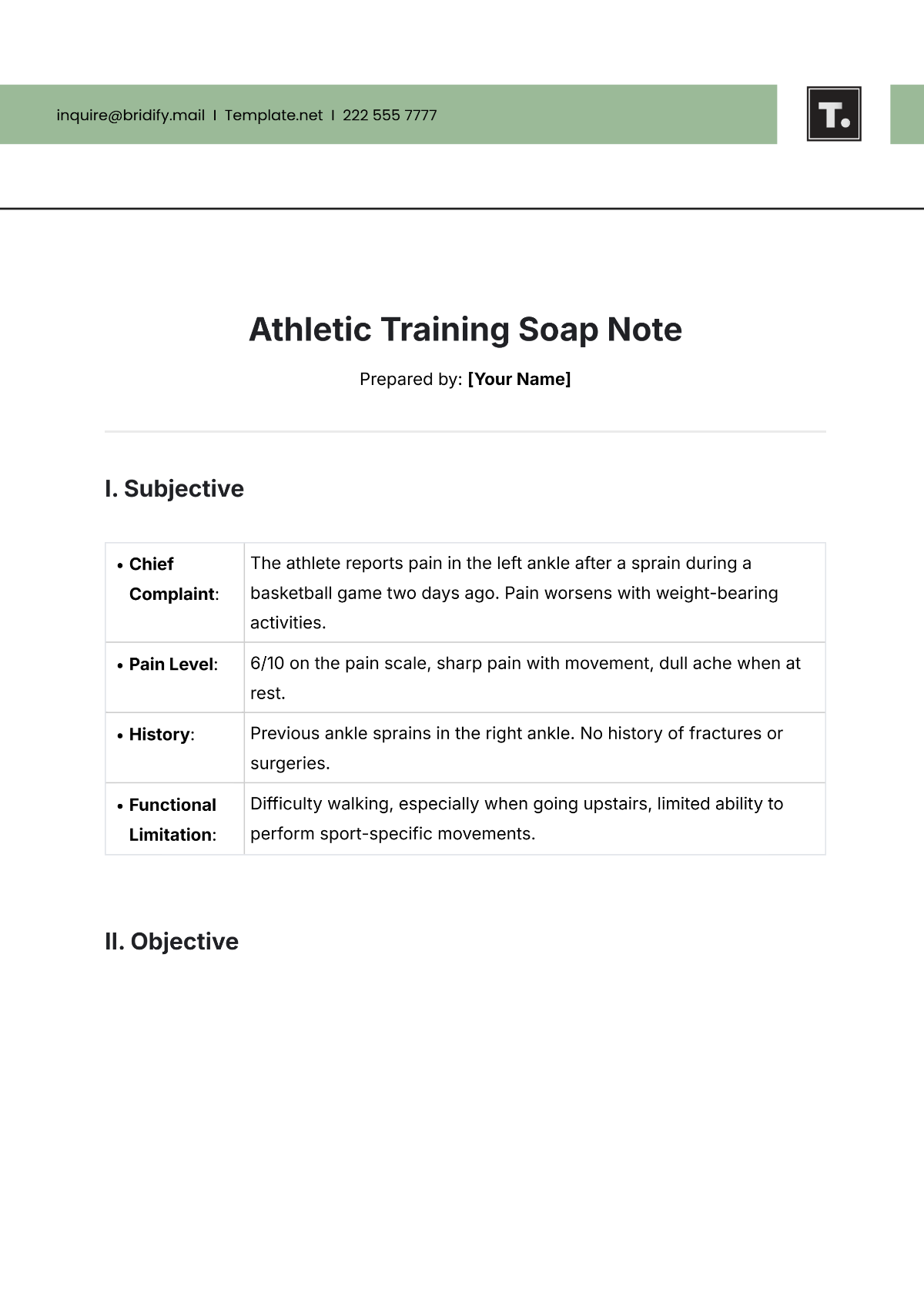
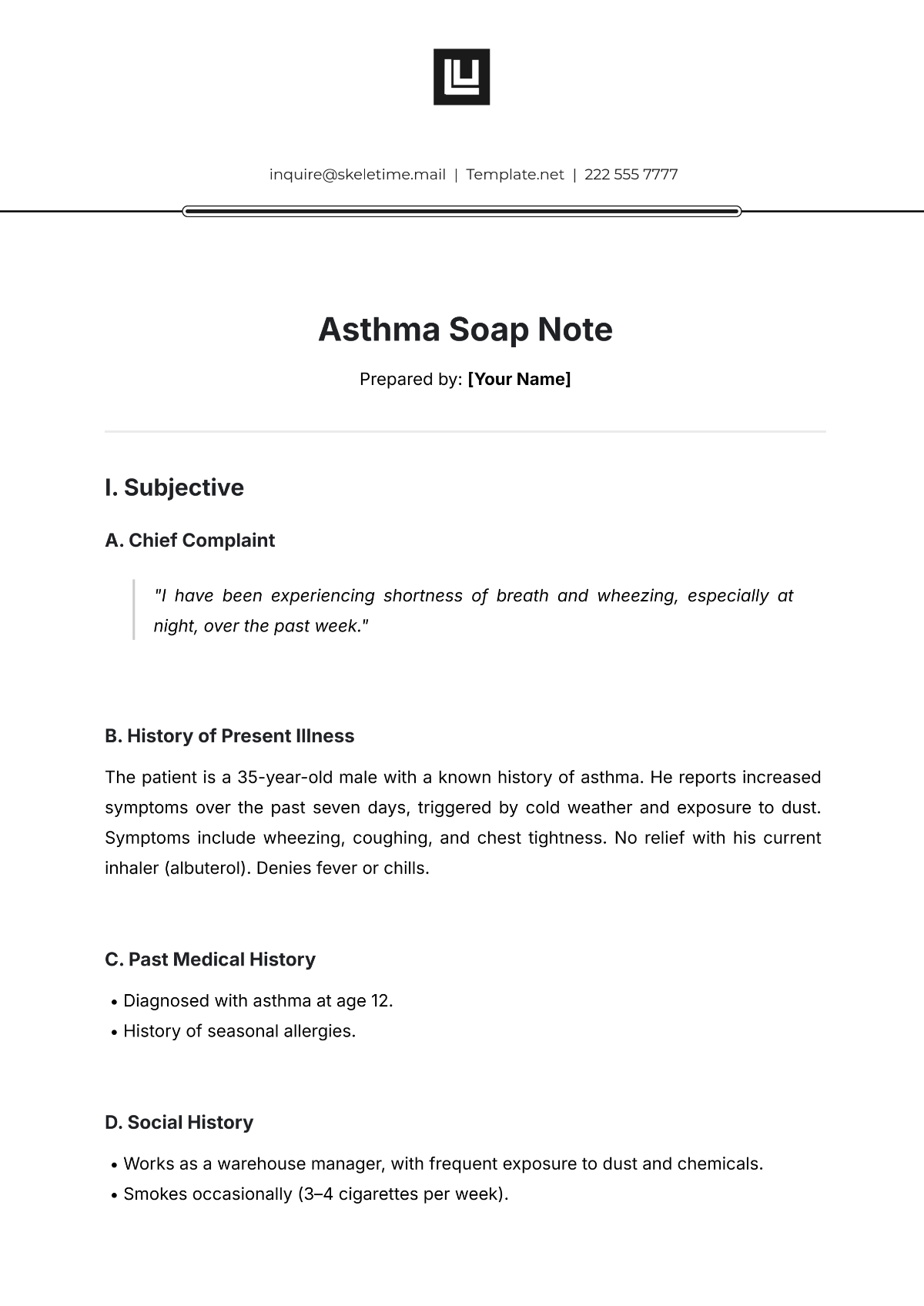
Blank Soap Note
Prepared by: [Your Name]
Date: ___________________
Patient Name: ______________________
DOB: ______________________
Medical Record Number: ______________________
I. Subjective
The patient's reported symptoms, concerns, and history
Chief Complaint (CC): ______________________________
History of Present Illness (HPI): ______________________________
Review of Systems (ROS): ______________________________
Past Medical History (PMH): ______________________________
Medications: ______________________________
Allergies: ______________________________
Social History (e.g., smoking, alcohol use): ______________________________
Family History: ______________________________
II. Objective
Clinician’s findings, including observations, vital signs, and examination results
Vital Signs:
Temperature: __________
Pulse: __________
Blood Pressure: __________
Respiratory Rate: __________
Oxygen Saturation: __________
Physical Exam:
General Appearance: ______________________________
HEENT (Head, Eyes, Ears, Nose, Throat): ______________________________
Cardiovascular: ______________________________
Respiratory: ______________________________
Abdominal: ______________________________
Musculoskeletal: ______________________________
Neurological: ______________________________
Laboratory/Diagnostic Results: ______________________________
Imaging: ______________________________
III. Assessment
Clinician’s interpretation based on subjective and objective data
Diagnosis/Clinical Impression: ______________________________
Differential Diagnosis: ______________________________
Severity: ______________________________
IV. Plan
Plan of action for further management
Treatment: ______________________________
Medications: ______________________________
Tests/Labs: ______________________________
Referrals: ______________________________
Follow-up: ______________________________
Patient Education: ______________________________

Name of Clinician: ______________________
Title: ______________________