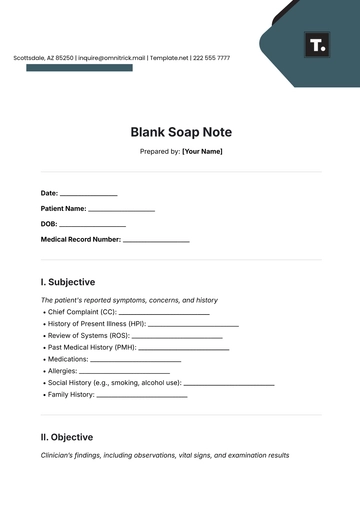
Free Medical Soap Note
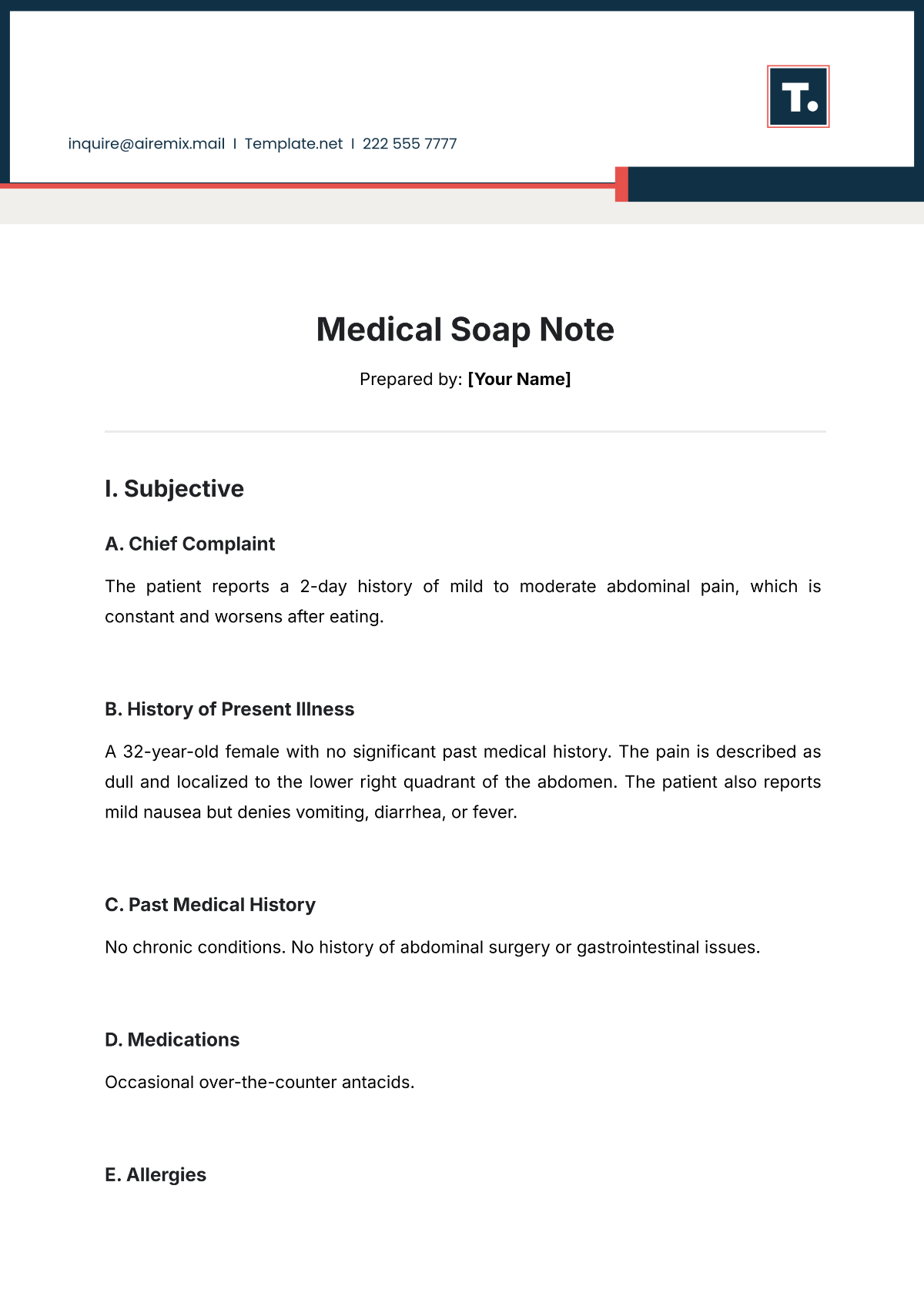
Prepared by: [Your Name]
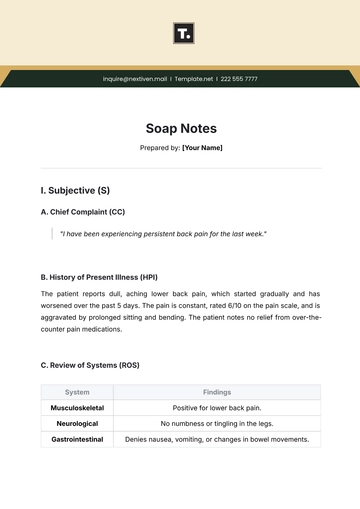
I. Subjective
A. Chief Complaint
The patient reports a 2-day history of mild to moderate abdominal pain, which is constant and worsens after eating.
B. History of Present Illness
A 32-year-old female with no significant past medical history. The pain is described as dull and localized to the lower right quadrant of the abdomen. The patient also reports mild nausea but denies vomiting, diarrhea, or fever.
C. Past Medical History
No chronic conditions. No history of abdominal surgery or gastrointestinal issues.
D. Medications
Occasional over-the-counter antacids.
E. Allergies
No known drug allergies.
F. Review of Systems
System | Findings |
|---|---|
Gastrointestinal | Positive for nausea. No vomiting, diarrhea, or constipation. |
Cardiovascular | No chest pain, palpitations, or edema. |
Respiratory | No shortness of breath, cough, or wheezing. |
Genitourinary | No urinary symptoms. |
II. Objective
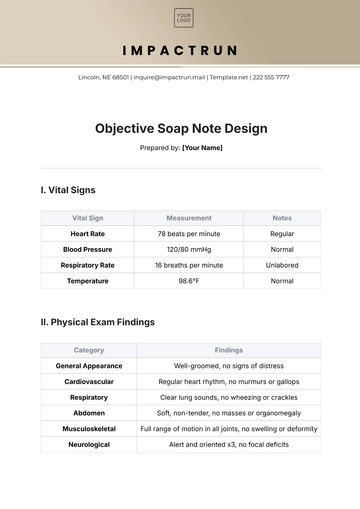
A. Vital Signs
Vital Sign | Measurement |
|---|---|
Blood Pressure | 120/80 mmHg |
Heart Rate | 76 bpm |
Respiratory Rate | 16 breaths/min |
Temperature | 98.6°F (37°C) |
Oxygen Saturation | 98% on room air |
B. Physical Examination
System | Findings |
|---|---|
General | Alert, well-nourished female in no acute distress. |
Abdomen | Tenderness to palpation in the right lower quadrant. |
No rebound tenderness or guarding. | |
Bowel sounds normal. | |
Other systems | Normal exam findings. |
C. Diagnostic Tests
None were performed at this visit.
III. Assessment
A. Differential Diagnosis
Acute appendicitis
Gastroenteritis
Irritable bowel syndrome (IBS)
B. Primary Diagnosis
Acute abdominal pain, possible early appendicitis.
IV. Plan
A. Further Testing
Order abdominal ultrasound to assess for signs of appendicitis. Consider a CT scan if symptoms worsen or remain unresolved.
B. Treatment
Prescribe pain management with acetaminophen.
Recommend clear liquids diet until symptoms resolve.
C. Follow-up
Follow up in 2-3 days or sooner if symptoms worsen. Advise the patient to seek immediate medical attention if pain becomes severe or if fever develops.
D. Patient Education
Educate the patient on signs of appendicitis and the importance of early intervention if symptoms change.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Enhance your clinical practice with Template.net's Medical Soap Note Template. Designed for healthcare efficiency, this template is both editable and customizable. It streamlines patient documentation, easily modified for precise detail using our Ai Editor Tool, making it an essential tool for accurate and efficient patient care records.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note