Chiropractic Soap Note
Prepared by: [Your Name]
I. Subjective
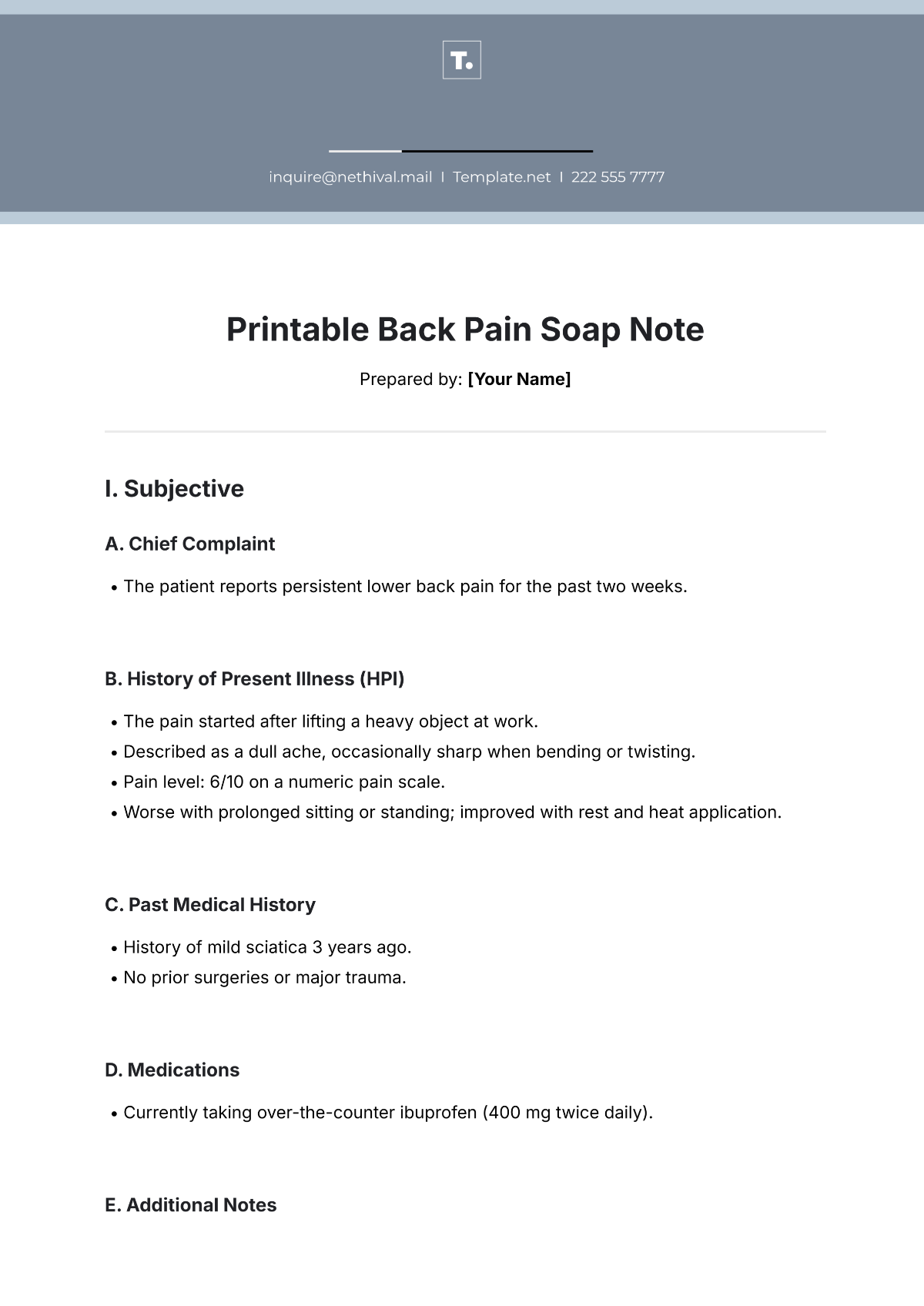
A. Patient-Reported Symptoms
The patient reports a dull ache in the lower back, rating the pain as 6/10 on the pain scale. The pain is aggravated by prolonged sitting and bending forward but improves with standing and walking. The patient states that the pain has been persistent for the past two weeks, with no significant improvement since the last visit.
B. Medical History
The patient has a history of lower back strain from a previous injury 6 months ago. No significant changes in general health or other medical conditions were reported.
C. Patient Goals
The patient expresses a desire to improve mobility and reduce pain in the lower back to resume normal activities such as walking and light exercise.
II. Objective
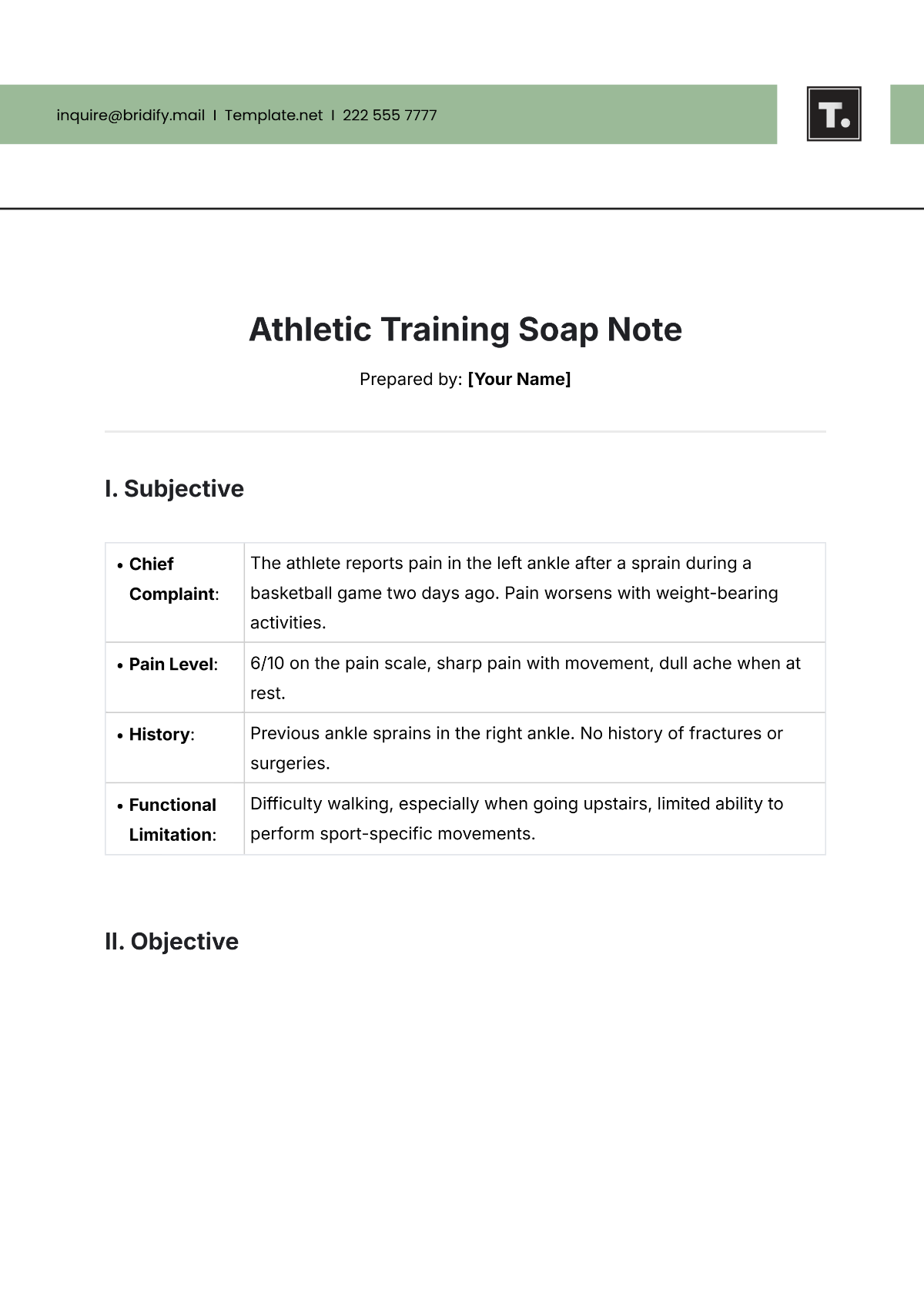
A. Observations
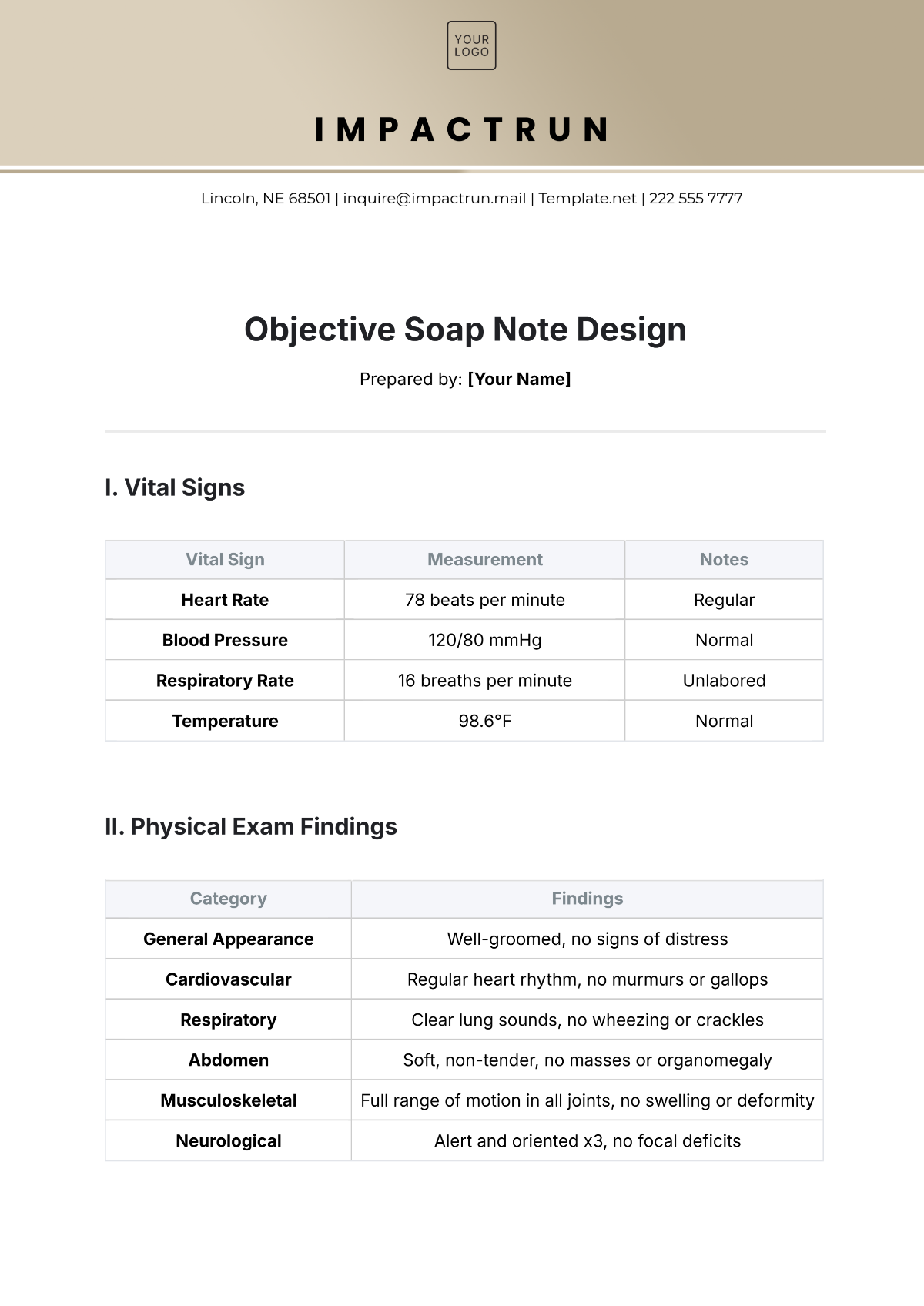
Observation | Details |
|---|---|
Posture | Slight forward head posture and increased lumbar lordosis. |
Gait | Slight limping was observed during walking due to lower back discomfort. |
Range of Motion | Limited lumbar flexion (50% of normal range), pain noted during flexion and extension. |
B. Physical Examination:
Examination Type | Findings |
|---|---|
Palpation | Tenderness was noted in the L4-L5 region with mild muscle spasms in the lower back. |
Neurological | Negative straight leg raise test; no signs of radiculopathy. |
C. Diagnostic Tests
X-ray results from the previous visit show mild degenerative changes in the lumbar spine but no evidence of fractures or herniated discs.
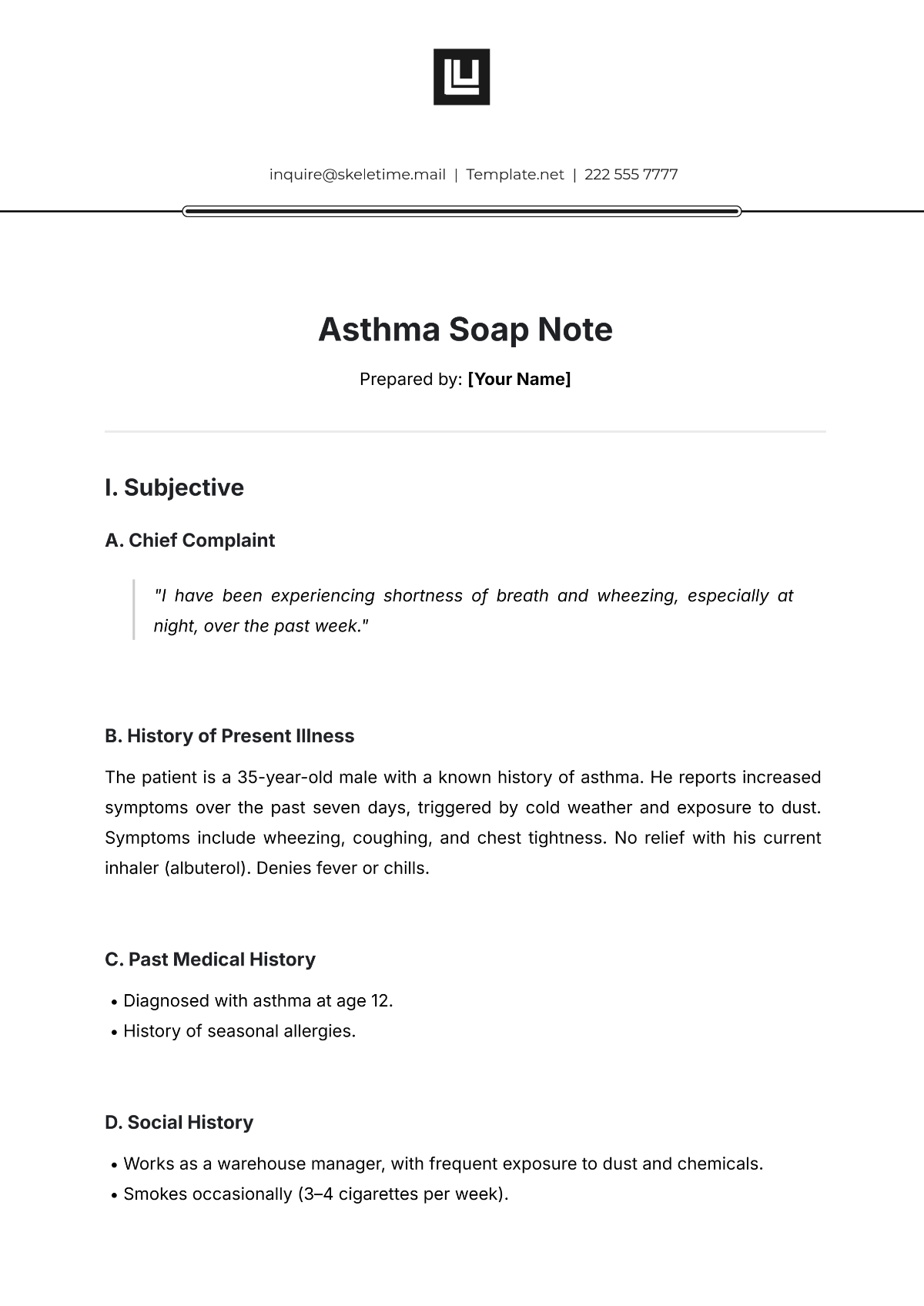
III. Assessment
A. Diagnosis
Chronic lower back strain with mild degenerative disc disease at L4-L5. The patient’s condition has shown slight improvement since the last visit but continues to be painful, especially with movement that stresses the lumbar spine.
B. Clinical Impression
The patient’s condition is consistent with mechanical low back pain due to muscle strain and spinal degeneration. The limited range of motion and pain suggest ongoing inflammation and muscle tightness.
IV. Plan
A. Treatment Plan
Chiropractic adjustments to the lumbar spine (L4-L5) to improve mobility.
Soft tissue therapy focuses on muscle relaxation and the reduction of spasms.
Home care instructions: Ice application for 20 minutes twice a day, avoid prolonged sitting, and perform gentle stretches for the lower back.
B. Follow-up
The patient is scheduled for a follow-up visit in one week to reassess symptoms and make any necessary adjustments to the treatment plan.