Free Internal Medicine Soap Note Layout
Prepared By: [Your Name]
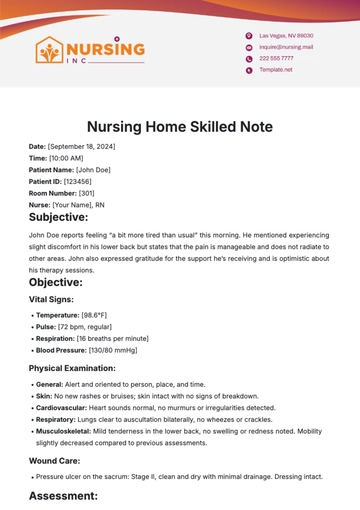
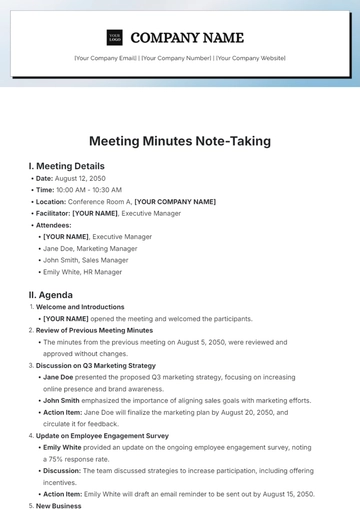
I. Subjective
A. Chief Complaint (CC)
A brief statement describing the primary reason for the patient’s visit, usually in the patient's own words.
B. History of Present Illness (HPI)
A detailed narrative of the onset, progression, duration, and characteristics of the patient’s symptoms, as well as any factors that exacerbate or alleviate them.
C. Past Medical History (PMH)
A summary of the patient’s previous medical conditions, surgeries, hospitalizations, and treatments.
D. Family History (FH)
Information about illnesses or conditions present in the patient’s immediate family may have genetic or hereditary relevance.
E. Social History (SH)
Details about the patient’s lifestyle, occupation, habits (e.g., smoking, alcohol use), and living conditions that may impact health.
F. Review of Systems (ROS)
A systematic review of body systems to identify any symptoms the patient may be experiencing, not directly related to the chief complaint.
II. Objective
A. Vital Signs
Measurements such as blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation.
B. Physical Examination (PE)
Findings from the healthcare provider’s inspection, palpation, auscultation, and other examination techniques for each relevant body system.
C. Laboratory and Diagnostic Results
Key results from blood tests, imaging studies, or other diagnostic procedures performed during or before the visit.
III. Assessment
A. Diagnosis
A concise statement of the patient’s condition(s), including differential diagnoses if applicable.
B. Clinical Impression
A summary of the healthcare provider’s interpretation of the findings, linking subjective and objective data.
IV. Plan
A. Treatment Plan
Specific actions for managing the patient’s condition(s), including prescribed medications, therapies, or procedures.
B. Patient Education
Instructions or guidance are provided to the patient about their condition, treatment, and follow-up.
C. Follow-Up
Details about when and how the patient should return for further evaluation or continued care.
D. Referrals
Recommendations for consultations with specialists or additional diagnostic evaluations if needed.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
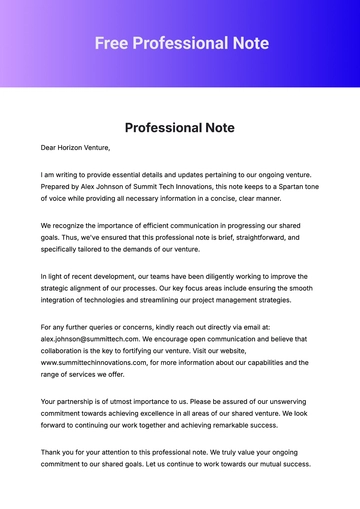
Optimize your internal medicine records with our Internal Medicine SOAP Note Layout Template at Template.net. This user-friendly, editable, and customizable template is perfect for capturing detailed medical evaluations and treatment plans. The professional layout ensures structured and comprehensive documentation. Personalize it easily using our AI Editor Tool, making it adaptable to your specific practice needs. Streamline your workflow while maintaining accuracy and professionalism with this ready-to-use template.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note