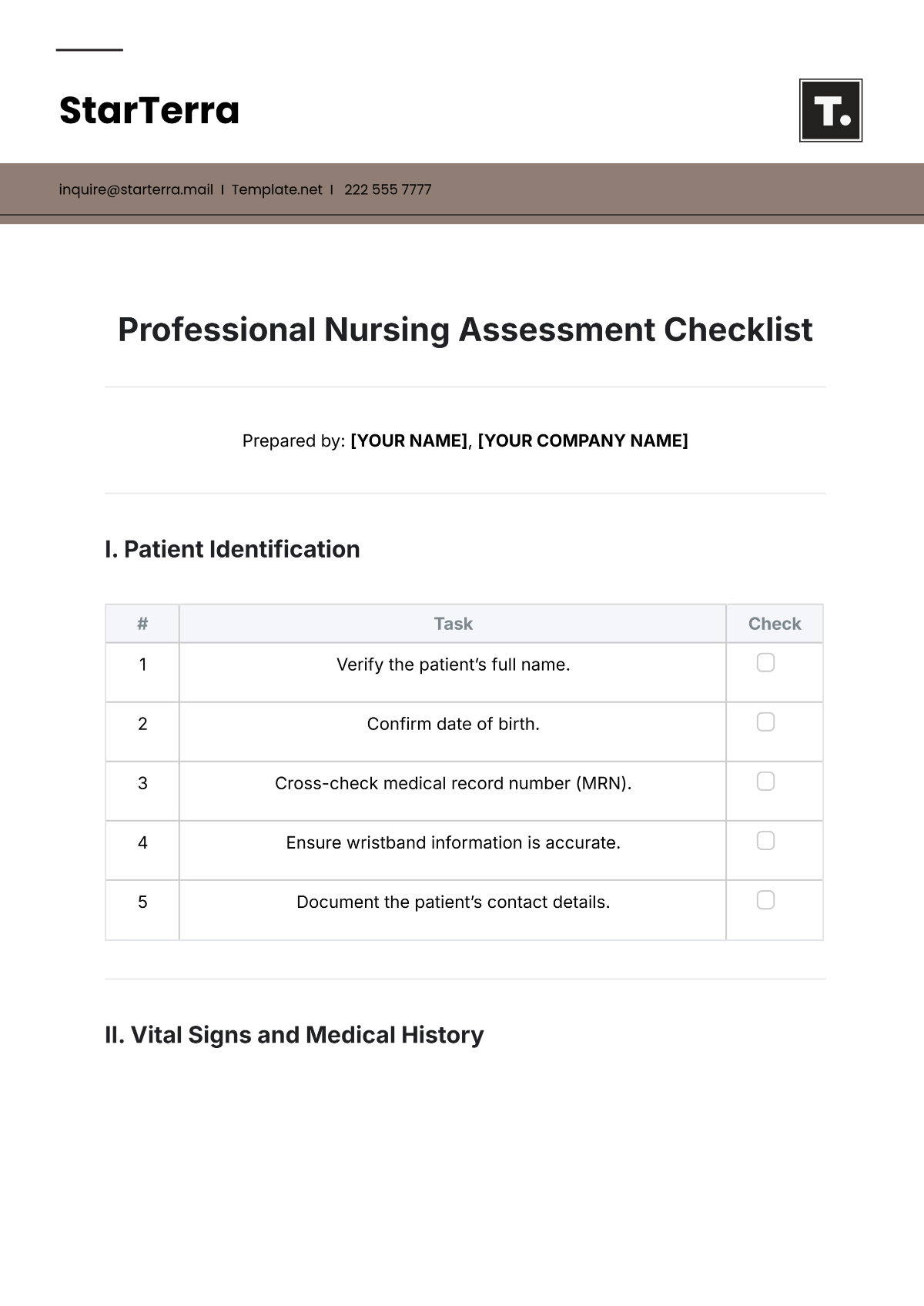
Free Professional Nursing Assessment Checklist
Uplift healthcare standards with our Nursing Assessment Checklist Template, available exclusively on Template.net. This highly editable and customizable tool streamlines nursing assessments for optimal patient care. Harness the power of our AI Editor Tool to effortlessly customize this checklist, ensuring precise and personalized assessments aligned with the highest healthcare standards.