Psychiatric Initial Evaluation
[YOUR COMPANY NAME]
Date: [INSERT DATE]
Introduction: This Performance Assessment Psychiatric Initial Evaluation aims to comprehensively assess an individual's performance across various domains relevant to mental health and well-being. It is designed to gather detailed information to aid in the understanding of the individual's functioning and identify areas of strength and potential areas for improvement.
Purpose: The Psychiatric Initial Evaluation evaluates a patient's mental health state through a detailed examination of their symptoms and medical history to conclude a diagnosis and treatment.
Instructions:
Assess each standard using the supplied rating scale and mark with a check (✔) as appropriate.
Evaluation:
Criteria Overview:
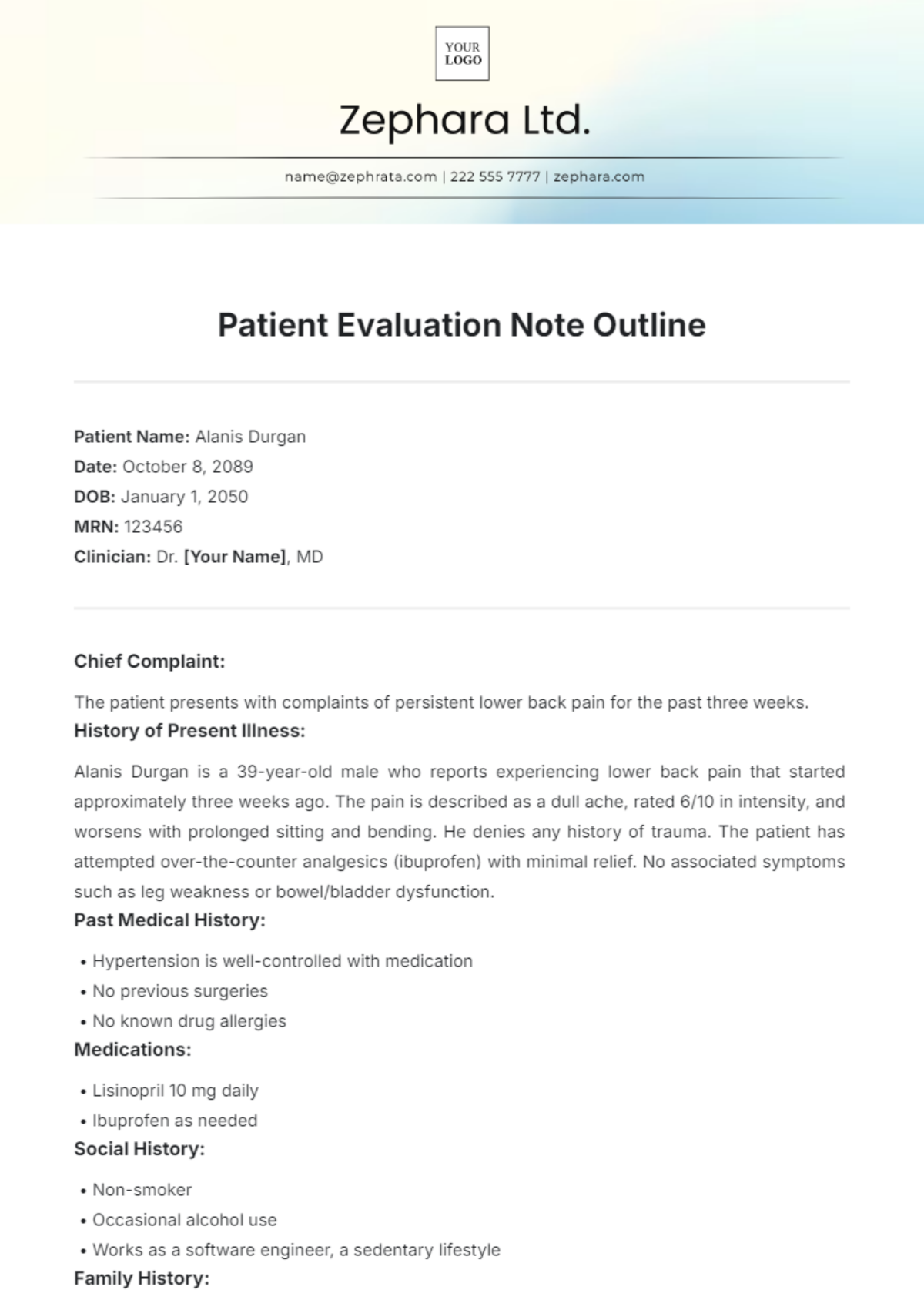
Asses patients for mental health concerns during their initial evaluation. It typically includes gathering information on the patient's psychiatric history, current symptoms, psychosocial stressors, and any previous treatments or medications. This evaluation aims to establish a comprehensive understanding of the patient's mental health status to guide further assessment and treatment planning.
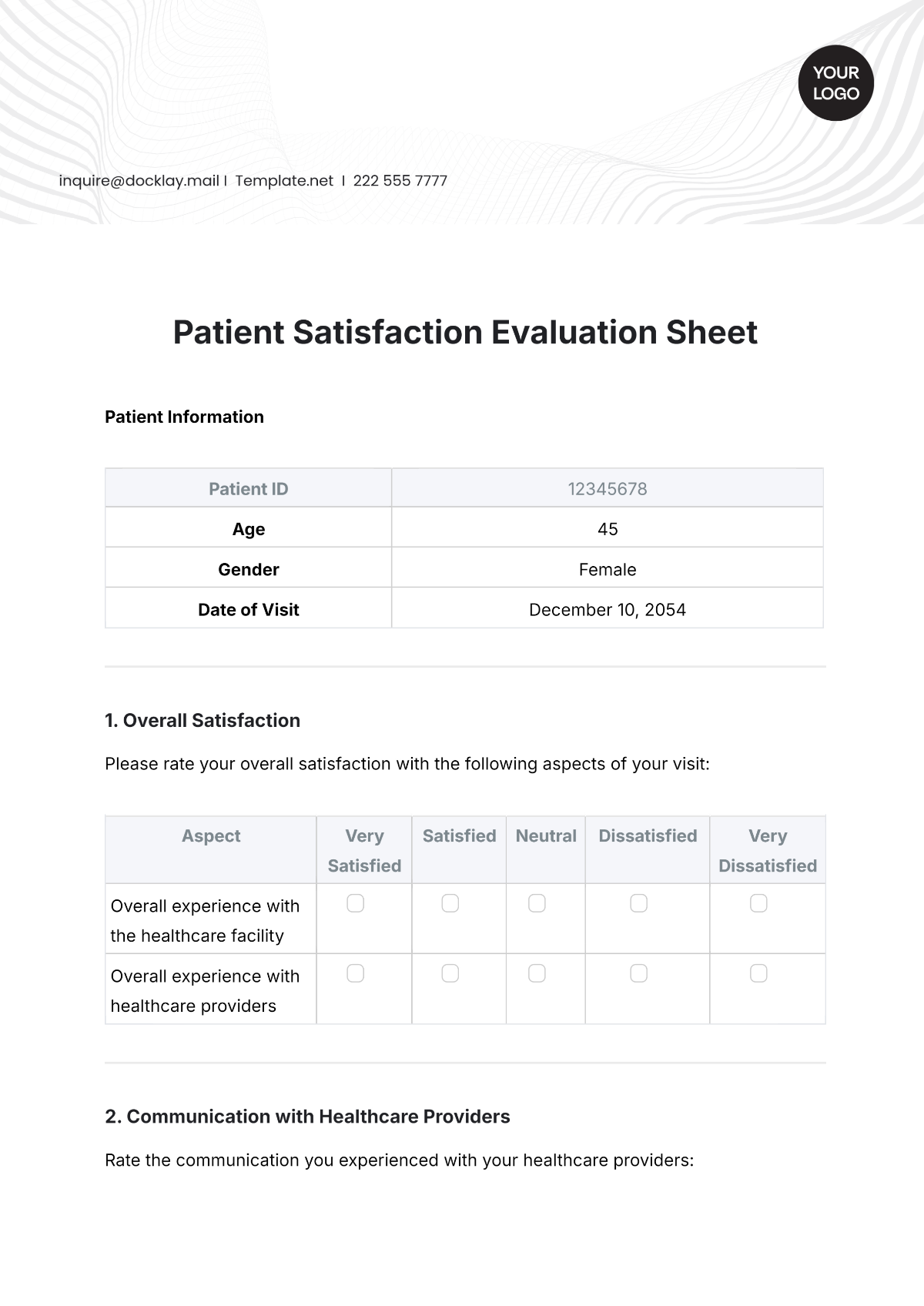
Patient History: The ability to provide accurate, detailed information about their personal and medical background. |
|---|
Rating Scale:
|
Mental Status Examination: The patient's mental acuity, perceptiveness, and level of consciousness. |
Rating Scale:
|
Symptoms: Verification of timestamp, severity, and impact of symptoms. |
|---|
Rating Scale:
|
Functional Assessment: Evaluation of the patient's ability to perform daily activities and tasks independently. |
|---|
Rating Scale:
|
Social Support Evaluation: Assessment of the patient's social network and support system. |
Rating Scale:
|
Additional Comments and Notes:
Comments and Notes |
|---|