Comprehensive Psychiatric Evaluation
[YOUR COMPANY NAME]
Date: [DATE]
Introduction:
This document is a comprehensive evaluation form designed to assess an individual's mental health status, including their emotional, behavioral, cognitive, and psychological functioning.
Overview:
It provides a range of parameters for assessment drawn by mental health professionals. This assessment forms the basis for formulating diagnoses and developing treatment plans.
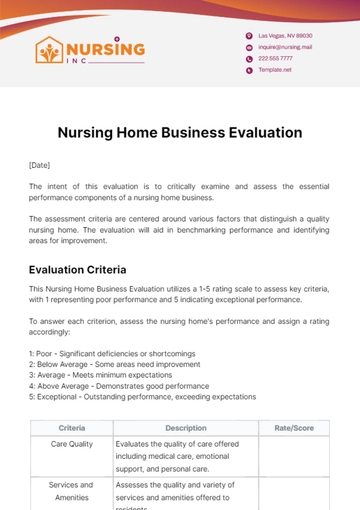
Criteria:
Evaluated areas include:
Client Intake - Initial client assessment involves collecting key details such as demographics, health history, past treatments, etc. It forms the basis for understanding the client's needs and guiding future evaluations.
Observation - Observation requires the clinician to keenly and objectively assess the client's activities, demeanor, and communication during the evaluation process, helping to pinpoint underlying patterns, symptoms, strengths, and issues not overtly reported by the client.
Behavioral Assessment - Behavioral assessment entails the systematic study and analysis of a client's behavior to identify possible psychological problems by observing aspects like mood changes, social behaviors, self-care, and task adherence instructions.
Cognitive Assessment - Cognitive assessment evaluates the client's cognition including attention, memory, problem-solving, language, and intellectual abilities using standardized tests to identify strengths and deficits.
Emotional Stability - Assessing emotional stability involves evaluating a client's ability to manage stress, regulate emotions, adapt to adversity, and maintain emotional balance.
Psychological Functioning- The psychological functioning assessment broadly examines a client's mental health and well-being, self-esteem, coping capacity, relationships, and adjustment. Clinicians use it to study symptoms, personality traits, and psychosocial functionality for a better client understanding of psychological health.
Overall Impression - This criterion is about the clinician's comprehensive analysis of the client, utilizing different assessment procedures to identify patterns, strengths, and concerns, and to form a general understanding of the client's psychological condition and requirements.
Recommended Treatment Plan -The suggested treatment plan includes a customized, scientifically-supported strategy for the client's unique needs, with potential elements like therapy modes, medication, lifestyle changes, patient education, and possibly referrals. The plan should be transparent, achievable, and cooperative, with the client participating in decision-making and objectives design.
For the rating scale, please note that:
1: Poor - Obvious challenges, requires immediate action
2: Fair - Mild challenges detected, intervention needed
3: Average - Normal functioning but with room for improvement
4: Good - Solid functioning, minor areas of improvement
5: Excellent - Healthy and appropriate functioning
Evaluation
Criteria | Description | Rating (1-5) |
|---|
Client Intake | Collection of comprehensive background data, personal history, and symptoms. | |
Observation | Assessment of the client's behavior, physical appearance, and interaction style during the session. | |
Behavioral Assessment | Evaluation of the client's actions, responses, and patterns of behavior | |
Cognitive Assessment | Evaluation of client's thinking patterns, problem-solving abilities, and overall mental processes. | |
Emotional Stability | Analysis of the client's emotional responses and control under varying circumstances. | |
Psychological Functioning | Examination of the client's mental health condition, including understanding and control of psychological reactions. | |
Overall Impression | General summary of the client's mental health status. | |
Recommended Treatment Plan | Proposed intervention strategy based on collected data and professional expertise. | |
Additional Comments and Notes
Evaluation Templates @ Template.net