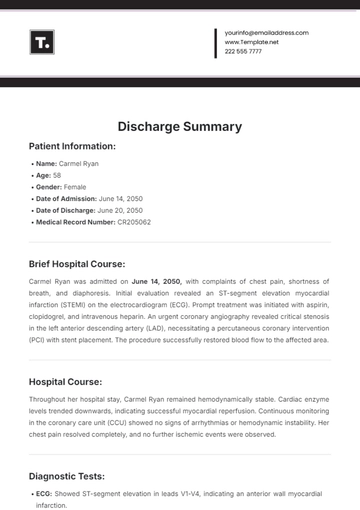
Free Nursing Discharge Summary
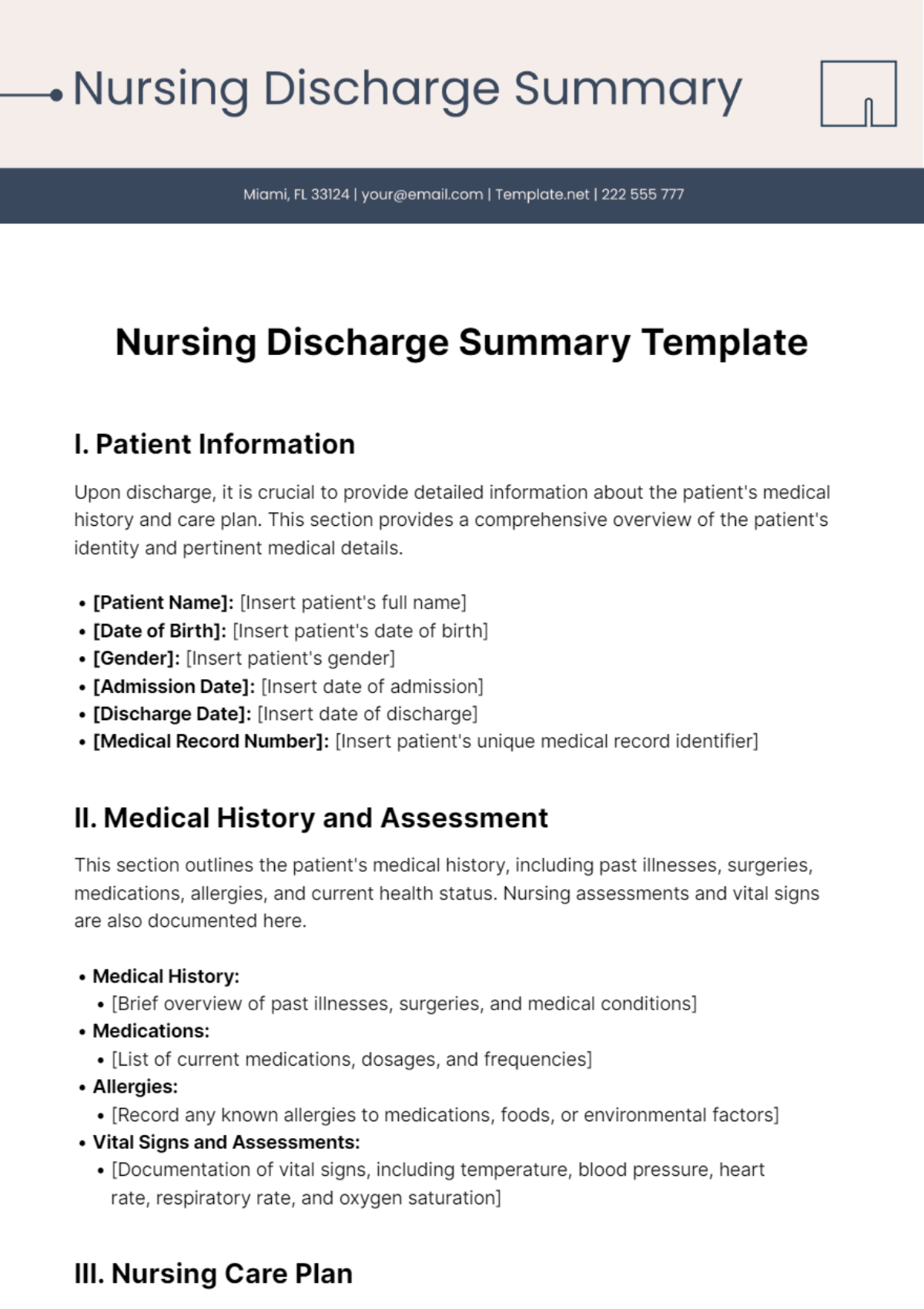
I. Patient Information
Upon discharge, it is crucial to provide detailed information about the patient's medical history and care plan. This section provides a comprehensive overview of the patient's identity and pertinent medical details.
[Patient Name]: [Insert patient's full name]
[Date of Birth]: [Insert patient's date of birth]
[Gender]: [Insert patient's gender]
[Admission Date]: [Insert date of admission]
[Discharge Date]: [Insert date of discharge]
[Medical Record Number]: [Insert patient's unique medical record identifier]
II. Medical History and Assessment
This section outlines the patient's medical history, including past illnesses, surgeries, medications, allergies, and current health status. Nursing assessments and vital signs are also documented here.
Medical History:
[Brief overview of past illnesses, surgeries, and medical conditions]
Medications:
[List of current medications, dosages, and frequencies]
Allergies:
[Record any known allergies to medications, foods, or environmental factors]
Vital Signs and Assessments:
[Documentation of vital signs, including temperature, blood pressure, heart rate, respiratory rate, and oxygen saturation]
III. Nursing Care Plan
This section outlines the nursing interventions and care provided to the patient during their hospitalization. It includes details such as nursing diagnoses, goals, interventions, and evaluations.
A. Nursing Diagnoses
[List of nursing diagnoses based on assessment findings]
B. Goals
[Specific and measurable goals set for each nursing diagnosis]
C. Interventions
[Detailed description of nursing interventions implemented to achieve goals]
D. Evaluation
[Assessment of patient response to nursing interventions and achievement of goals]
IV. Discharge Instructions
Clear and concise discharge instructions are provided to ensure the patient understands their care plan post-discharge. This section includes information on medications, follow-up appointments, activity restrictions, diet, and self-care.
Medication Instructions:
[List of medications prescribed upon discharge, including dosages and frequencies]
Follow-up Appointments:
[Details of scheduled follow-up appointments with healthcare providers]
Activity Restrictions:
[Guidance on limitations on physical activities and recommendations for gradual resumption]
Dietary Guidelines:
[Instructions regarding dietary restrictions or modifications]
Self-care Instructions:
[Guidance on wound care, medication management, and symptom monitoring]
V. Conclusion
In conclusion, this Nursing Discharge Summary Template serves as a comprehensive document summarizing key information about the patient's hospitalization and post-discharge care plan from a nursing perspective. By adhering to standardized formats and including essential sections such as [Patient Information], [Medical History and Assessment], [Nursing Care Plan], and [Discharge Instructions], healthcare providers can ensure clarity, accuracy, and continuity of care for the patient. Effective utilization of this template facilitates communication among healthcare team members and empowers patients to actively participate in their recovery process.
Summarized By: [YOUR NAME]
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Introducing the Nursing Discharge Summary Template from Template.net, your comprehensive solution for efficient patient care documentation. This editable and customizable resource ensures precision in summarizing nursing care. Seamlessly tailor summaries to individual patient needs with our AI Editor Tool, streamlining discharge processes for optimal patient outcomes.