Altered Gas Exchange Case Study
I. Introduction
The introduction section of the Altered Gas Exchange Case Study provides an overview of the patient's condition, relevant background information, and the purpose of the case study.
A. Background Information
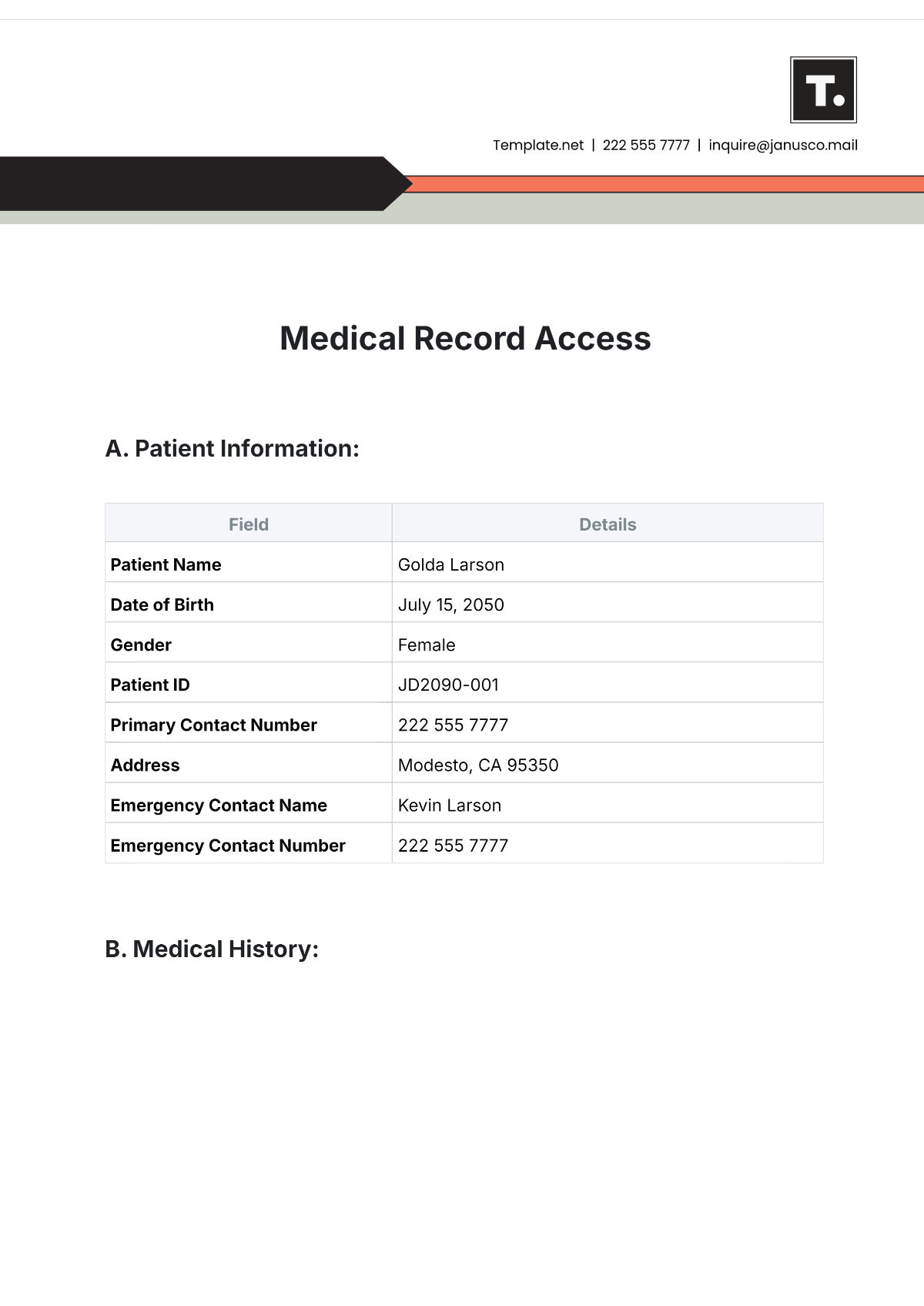
Patient Name: [Patient Name]
Age: [Age]
Gender: [Gender]
[Patient Name] presented to the emergency department complaining of progressive dyspnea, cough, and increased sputum production over the past week. He has a medical history of chronic obstructive pulmonary disease (COPD) and hypertension. He is currently taking an albuterol inhaler as needed for COPD exacerbations and lisinopril for hypertension.
B. Purpose
The purpose of this case study is to analyze the patient's altered gas exchange condition, identify contributing factors, and develop an effective management plan to improve respiratory function and overall patient outcomes.
II. Patient History
This section delves into the patient's medical history, including past illnesses, surgeries, lifestyle factors, and current medications.
A. Medical History
Past Illnesses:
COPD exacerbations requiring hospitalization twice in the past year.
Surgeries:
None
Lifestyle Factors:
Former smoker (quit 10 years ago), sedentary lifestyle.
B. Current Medications
The patient is currently taking the following medications:
Medication Name | Dosage | Frequency | Route |
|---|---|---|---|
Albuterol Inhaler | As needed | PRN | Inhalation |
Lisinopril | 10 mg | Daily | Oral |
III. Assessment Findings
In this section, the assessment findings related to altered gas exchange are documented, including physical examination results, diagnostic tests, and laboratory findings.
A. Physical Examination
Vital Signs:
Respiratory rate: 24 breaths/min
Oxygen saturation: 88% on room air
Respiratory Assessment:
Diminished breath sounds with prolonged expiration, use of accessory muscles, and tripod positioning.
B. Diagnostic Tests
Arterial Blood Gas (ABG):
pH: 7.32
PaO2: 55 mmHg
PaCO2: 58 mmHg
HCO3: 28 mEq/L
Pulmonary Function Tests (PFTs):
FEV1: 45% predicted
FVC: 60% predicted
DLCO: 50% predicted
IV. Nursing Diagnosis
Based on the assessment findings, nursing diagnoses are formulated to guide patient care and interventions.
A. Impaired Gas Exchange related to COPD exacerbation as evidenced by hypoxemia and hypercapnia.
B. Ineffective Airway Clearance related to increased sputum production and bronchoconstriction as evidenced by diminished breath sounds and prolonged expiration.
V. Plan of Care
This section outlines the interdisciplinary plan of care tailored to address the patient's altered gas exchange.
A. Goals
Short-term Goals:
Improve oxygenation to achieve PaO2 > 60 mmHg.
Reduce hypercapnia to achieve PaCO2 < 50 mmHg.
Long-term Goals:
Optimize respiratory function to minimize COPD exacerbations and improve quality of life.
B. Interventions
Oxygen Therapy:
Initiate supplemental oxygen therapy at 2 L/min via nasal cannula to maintain oxygen saturation > 90%.
Airway Clearance Techniques:
Encourage deep breathing exercises and the use of incentive spirometry to promote airway clearance.
Administer nebulized bronchodilators (e.g., albuterol) and mucolytics (e.g., acetylcysteine) as prescribed.
VI. Evaluation
The evaluation section assesses the effectiveness of the interventions implemented and the patient's response to treatment.
A. Outcomes
Improvement in Oxygenation:
Follow-up ABG shows improvement in PaO2 to 65 mmHg on supplemental oxygen.
Resolution of Respiratory Symptoms:
Diminished dyspnea was reported by the patient, with decreased use of accessory muscles and improved breath sounds.
B. Reassessment
Repeat Diagnostic Tests:
Plan for repeat ABG in 24 hours to evaluate further improvement in gas exchange.
Patient Feedback:
The patient expresses satisfaction with symptom relief and understanding of self-management strategies for COPD exacerbations.
VII. Conclusion
In conclusion, the management of altered gas exchange in patients with chronic respiratory conditions such as COPD requires a comprehensive approach that addresses both the underlying pathology and acute exacerbations. Through diligent assessment, targeted interventions, and close monitoring, significant improvements in respiratory function and symptom relief can be achieved. This case study highlights the importance of individualized care plans tailored to the patient's specific needs and emphasizes the role of interdisciplinary collaboration in optimizing patient outcomes. Moving forward, ongoing education and support for patients with chronic respiratory diseases are essential to empower them to manage their condition effectively and improve their overall quality of life.
Prepared by:
[Your Name]
[Your Position]
[Your Company Name]
Contact Details:
[Your Company Email]
[Your Company Number]