Free Medical Incident Report
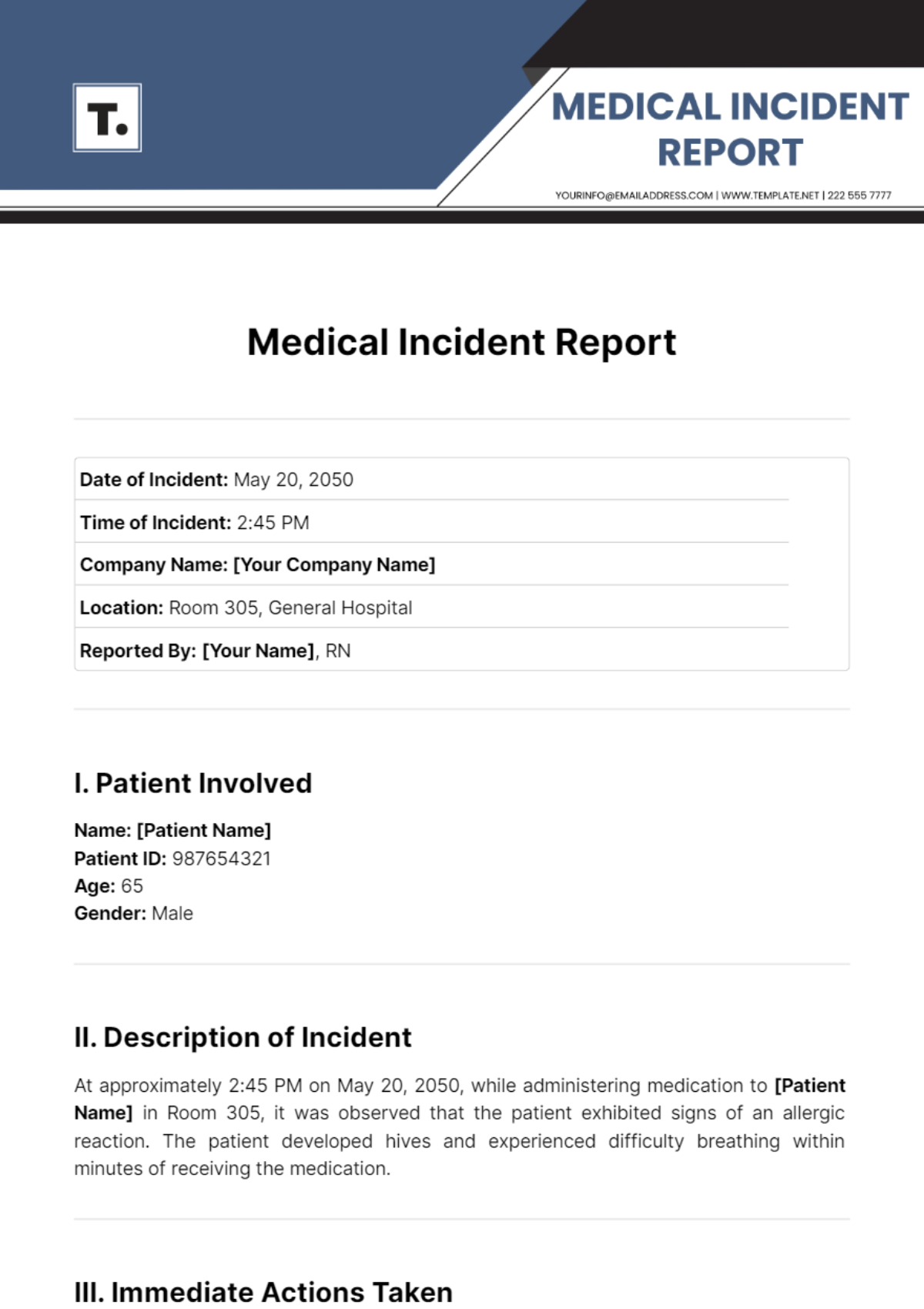
Date of Incident: May 20, 2050 |
Time of Incident: 2:45 PM |
Company Name: [Your Company Name] |
Location: Room 305, General Hospital |
Reported By: [Your Name], RN |
I. Patient Involved
Name: [Patient Name]
Patient ID: 987654321
Age: 65
Gender: Male
II. Description of Incident
At approximately 2:45 PM on May 20, 2050, while administering medication to [Patient Name] in Room 305, it was observed that the patient exhibited signs of an allergic reaction. The patient developed hives and experienced difficulty breathing within minutes of receiving the medication.
III. Immediate Actions Taken
Medication Administration Halted: Upon noticing the symptoms, the administration of the medication was immediately stopped.
Emergency Response Initiated: The Rapid Response Team was notified, and they arrived within 3 minutes.
Administered Treatment: Epinephrine was administered, and the patient was given oxygen.
Monitoring: The patient was closely monitored for any further reactions.
IV. Incident Analysis
A. Cause of Incident
Initial investigation suggests that the allergic reaction may have been caused by the medication administered, which was Ceftriaxone. The patient's chart indicated a known allergy to penicillin, but there was no documented cross-reactivity to Ceftriaxone.
B. Contributing Factors
Documentation Gap: The patient's allergy profile may not have been comprehensively updated.
Communication Breakdown: Potential failure in communication between the healthcare providers regarding the patient's allergy history.
V. Follow-Up Actions
Patient Monitoring: Continuous monitoring of the patient's condition in the ICU for the next 24 hours.
Review of Allergy Documentation: A thorough review and update of the patient's medical records to ensure all allergies are accurately documented.
Staff Training: Implementation of a refresher course for all healthcare providers on the importance of reviewing patient allergy information before administering any medication.
Incident Review Meeting: A meeting is scheduled with the healthcare team involved to discuss the incident and identify measures to prevent future occurrences.
VI. Witness Statements
Witness 1:
Name: Dr. Emily Johnson
Position: Attending Physician
Statement: "Upon arrival, the patient was in respiratory distress. Immediate administration of epinephrine was necessary, and the patient's condition stabilized shortly after."
Witness 2:
Name: Mark Lee
Position: Pharmacist
Statement: "The prescribed medication was Ceftriaxone, typically considered safe unless contraindicated by specific allergies, which in this case was not adequately cross-referenced."
VII. Recommendations
Enhanced Screening: Implement a mandatory double-check system for allergy verification before medication administration.
Improved Communication: Establish a protocol for mandatory verbal confirmation of patient allergies during shift changes.
Technological Support: Utilize electronic health record (EHR) systems more effectively to flag potential allergy interactions in real-time.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
A Medical Incident Report is a detailed document that records an unexpected event or situation within a healthcare setting, such as a hospital, clinic, or nursing home, that may have caused harm or had the potential to cause harm to a patient, staff member, or visitor. These reports are crucial for identifying, analyzing, and mitigating risks to improve safety and quality of care.
You may also like
- Sales Report
- Daily Report
- Project Report
- Business Report
- Weekly Report
- Incident Report
- Annual Report
- Report Layout
- Report Design
- Progress Report
- Marketing Report
- Company Report
- Monthly Report
- Audit Report
- Status Report
- School Report
- Reports Hr
- Management Report
- Project Status Report
- Handover Report
- Health And Safety Report
- Restaurant Report
- Construction Report
- Research Report
- Evaluation Report
- Investigation Report
- Employee Report
- Advertising Report
- Weekly Status Report
- Project Management Report
- Finance Report
- Service Report
- Technical Report
- Meeting Report
- Quarterly Report
- Inspection Report
- Medical Report
- Test Report
- Summary Report
- Inventory Report
- Valuation Report
- Operations Report
- Payroll Report
- Training Report
- Job Report
- Case Report
- Performance Report
- Board Report
- Internal Audit Report
- Student Report
- Monthly Management Report
- Small Business Report
- Accident Report
- Call Center Report
- Activity Report
- IT and Software Report
- Internship Report
- Visit Report
- Product Report
- Book Report
- Property Report
- Recruitment Report
- University Report
- Event Report
- SEO Report
- Conference Report
- Narrative Report
- Nursing Home Report
- Preschool Report
- Call Report
- Customer Report
- Employee Incident Report
- Accomplishment Report
- Social Media Report
- Work From Home Report
- Security Report
- Damage Report
- Quality Report
- Internal Report
- Nurse Report
- Real Estate Report
- Hotel Report
- Equipment Report
- Credit Report
- Field Report
- Non Profit Report
- Maintenance Report
- News Report
- Survey Report
- Executive Report
- Law Firm Report
- Advertising Agency Report
- Interior Design Report
- Travel Agency Report
- Stock Report
- Salon Report
- Bug Report
- Workplace Report
- Action Report
- Investor Report
- Cleaning Services Report
- Consulting Report
- Freelancer Report
- Site Visit Report
- Trip Report
- Classroom Observation Report
- Vehicle Report
- Final Report
- Software Report