Free Medical Emergency Incident Report
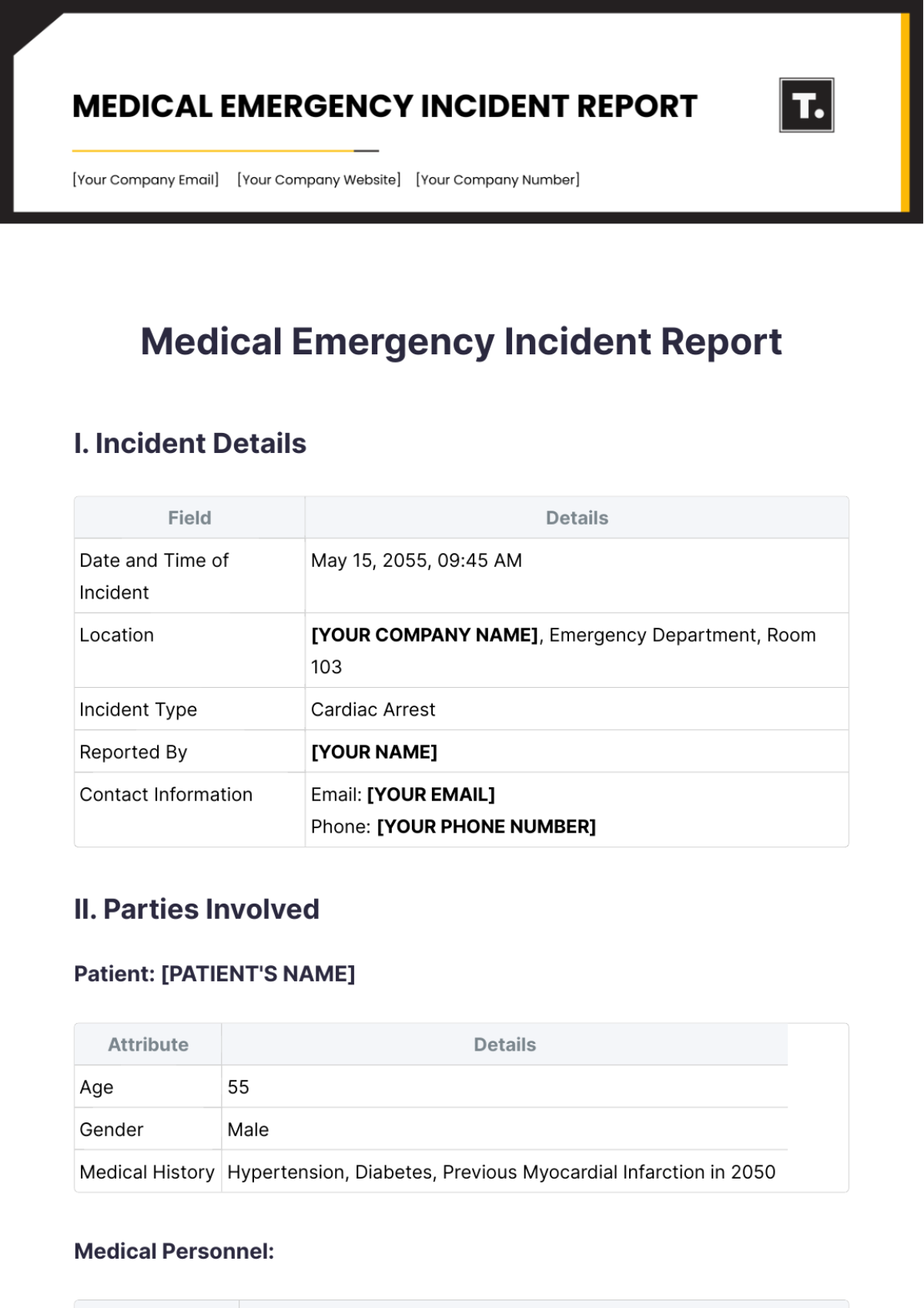
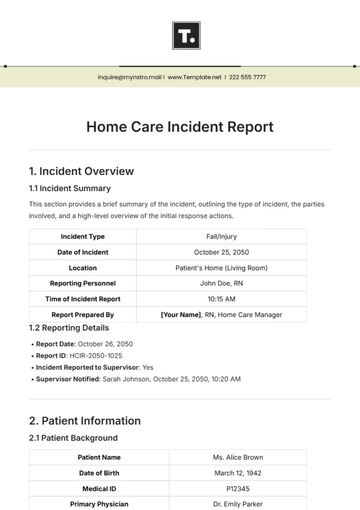
I. Incident Details
Field | Details |
|---|---|
Date and Time of Incident | May 15, 2055, 09:45 AM |
Location | [YOUR COMPANY NAME], Emergency Department, Room 103 |
Incident Type | Cardiac Arrest |
Reported By | [YOUR NAME] |
Contact Information | Email: [YOUR EMAIL] Phone: [YOUR PHONE NUMBER] |
II. Parties Involved
Patient: [PATIENT'S NAME]
Attribute | Details |
|---|---|
Age | 55 |
Gender | Male |
Medical History | Hypertension, Diabetes, Previous Myocardial Infarction in 2050 |
Medical Personnel:
Name | Role |
|---|---|
[PHYSICIAN'S NAME] | Emergency Physician - Directed resuscitation efforts, coordinated with the nursing staff |
[NURSE'S NAME] | Registered Nurse - Assisted with CPR, fetched defibrillator, documented vital signs |
III. Description of Events
The incident occurred in the waiting area of the emergency department. [PATIENT'S NAME] was initially observed sitting in a chair, complaining of chest pain. Suddenly, he collapsed, losing consciousness and ceasing to breathe. [YOUR NAME], who was nearby, quickly assessed the situation and initiated CPR while [NURSE'S NAME] called for assistance and fetched the defibrillator.
Upon arrival, medical personnel found the patient unresponsive with absent breathing and pulse. CPR was continued while [PHYSICIAN'S NAME] directed the resuscitation efforts. After the first cycle of CPR, the defibrillator was applied, delivering one shock for ventricular fibrillation. CPR was resumed immediately post-shock. After the second cycle of CPR, spontaneous circulation returned, and the patient regained a pulse and spontaneous respirations.
IV. Medical Assessment
Vital Signs | Upon Arrival | Post-Resuscitation |
|---|---|---|
Heart Rate (bpm) | 0 | 110 |
Blood Pressure (mmHg) | Unmeasurable | 130/80 |
Respiratory Rate (bpm) | 0 | 20 |
Medical Evaluation:
ECG showed ventricular fibrillation initially, followed by sinus rhythm post-defibrillation. No ST-segment changes were observed.
V. Outcome
Current Condition: [PATIENT'S NAME] was stabilized and transferred to the Cardiac Intensive Care Unit (CICU) for further monitoring and treatment.
Transportation: The patient was transferred to the CICU via hospital bed, accompanied by nursing staff.
Follow-up Care: Cardiology consult scheduled for further evaluation and consideration of coronary angiography.
VI. Supporting Documentation
Medical Records: ECG strips, vital signs chart, nursing notes.
Photographs/Visuals: None
VII. Incident Analysis
Root Cause Analysis: Myocardial infarction (MI) leading to ventricular fibrillation is presumed as the underlying cause, given the patient's history of hypertension, diabetes, and previous MI.
Preventive Measures: Recommend regular cardiac monitoring for high-risk patients in the emergency department, and ensuring the availability of trained personnel and equipment for prompt response to cardiac emergencies.
VIII. Legal and Compliance Considerations
Regulatory Compliance: Hospital policies and procedures for emergency response followed, including documentation and reporting requirements.
Legal Implications: No legal implications identified at this time. Patient care is provided in accordance with established standards and guidelines.
IX. Lessons Learned
Key Takeaways: Prompt initiation of CPR and defibrillation significantly improved patient outcomes. Effective teamwork and communication among medical staff were crucial in the successful resuscitation of the patient.
Training Needs: Ongoing CPR and ACLS training for all healthcare staff to maintain competency in emergency response protocols.
X. Conclusion
The swift and coordinated response by hospital staff led to successful resuscitation and stabilization of the patient. Recommendations for preventive measures and ongoing training have been made to ensure continued readiness for similar emergencies.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Ensure accurate documentation with the Medical Emergency Incident Report Template from Template.net. This fully customizable and editable template simplifies reporting, saving time and effort. Utilize our AI Editor Tool for precise, professional reports every time. Ideal for healthcare professionals, this template guarantees comprehensive incident records, enhancing your emergency response efficiency.
You may also like
- Sales Report
- Daily Report
- Project Report
- Business Report
- Weekly Report
- Incident Report
- Annual Report
- Report Layout
- Report Design
- Progress Report
- Marketing Report
- Company Report
- Monthly Report
- Audit Report
- Status Report
- School Report
- Reports Hr
- Management Report
- Project Status Report
- Handover Report
- Health And Safety Report
- Restaurant Report
- Construction Report
- Research Report
- Evaluation Report
- Investigation Report
- Employee Report
- Advertising Report
- Weekly Status Report
- Project Management Report
- Finance Report
- Service Report
- Technical Report
- Meeting Report
- Quarterly Report
- Inspection Report
- Medical Report
- Test Report
- Summary Report
- Inventory Report
- Valuation Report
- Operations Report
- Payroll Report
- Training Report
- Job Report
- Case Report
- Performance Report
- Board Report
- Internal Audit Report
- Student Report
- Monthly Management Report
- Small Business Report
- Accident Report
- Call Center Report
- Activity Report
- IT and Software Report
- Internship Report
- Visit Report
- Product Report
- Book Report
- Property Report
- Recruitment Report
- University Report
- Event Report
- SEO Report
- Conference Report
- Narrative Report
- Nursing Home Report
- Preschool Report
- Call Report
- Customer Report
- Employee Incident Report
- Accomplishment Report
- Social Media Report
- Work From Home Report
- Security Report
- Damage Report
- Quality Report
- Internal Report
- Nurse Report
- Real Estate Report
- Hotel Report
- Equipment Report
- Credit Report
- Field Report
- Non Profit Report
- Maintenance Report
- News Report
- Survey Report
- Executive Report
- Law Firm Report
- Advertising Agency Report
- Interior Design Report
- Travel Agency Report
- Stock Report
- Salon Report
- Bug Report
- Workplace Report
- Action Report
- Investor Report
- Cleaning Services Report
- Consulting Report
- Freelancer Report
- Site Visit Report
- Trip Report
- Classroom Observation Report
- Vehicle Report
- Final Report
- Software Report