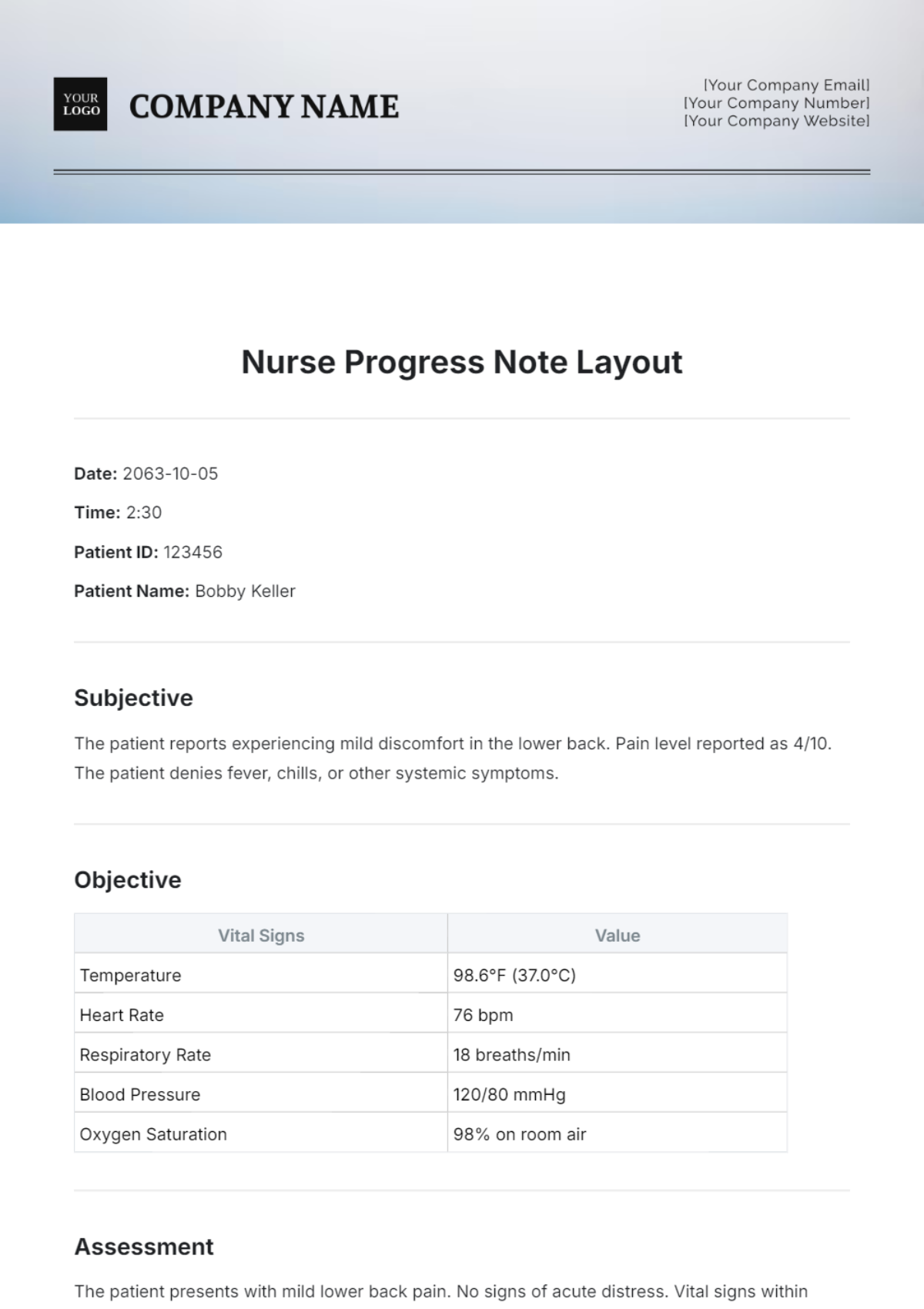
Nurse Progress Note Layout
Date: 2063-10-05
Time: 2:30
Patient ID: 123456
Patient Name: Bobby Keller
Subjective
The patient reports experiencing mild discomfort in the lower back. Pain level reported as 4/10. The patient denies fever, chills, or other systemic symptoms.
Objective
Vital Signs | Value |
|---|---|
Temperature | 98.6°F (37.0°C) |
Heart Rate | 76 bpm |
Respiratory Rate | 18 breaths/min |
Blood Pressure | 120/80 mmHg |
Oxygen Saturation | 98% on room air |
Assessment
The patient presents with mild lower back pain. No signs of acute distress. Vital signs within normal limits.
Plan
Administer acetaminophen 500 mg orally every 6 hours as needed for pain.
Encourage the patient to apply a warm compress to the lower back.
Advise the patient to avoid heavy lifting and strenuous activities.
Schedule a follow-up appointment in one week.
Instruct the patient to return if symptoms worsen or new symptoms arise.
Signature: Nurse [YOUR NAME], RN
Date: 2063-10-05