Simple Healthcare Protocol
Objective:
To provide a clear and concise protocol for the assessment and management of fever in adult patients.
Scope:
This protocol applies to all healthcare providers at [Your Company Name], including nurses, physicians, and physician assistants, who are responsible for the care of adult patients presenting with fever.
1. Initial Assessment
Measure Temperature:
Use a digital thermometer to record the patient's temperature orally.
If oral temperature is not feasible, use a tympanic, rectal, or axillary method.
Patient History:
Ask the patient about the onset, duration, and any associated symptoms (e.g., chills, sweating, headache).
Inquire about recent travel, exposure to infectious diseases, and any use of medications (e.g., antipyretics).
Physical Examination:
Check for signs of infection, such as rash, swollen lymph nodes, or localized pain.
Assess the patient’s vital signs, including heart rate, blood pressure, and respiratory rate.
2. Management
If Temperature is Below 38°C (100.4°F):
Encourage fluid intake to prevent dehydration.
Reassess the patient’s condition after 2 hours.
No immediate intervention required unless symptoms worsen.
If Temperature is Between 38°C and 39°C (100.4°F - 102.2°F):
Administer acetaminophen or ibuprofen as per dosage guidelines, if no contraindications.
Encourage fluid intake and rest.
Monitor temperature every 4 hours.
If Temperature is Above 39°C (102.2°F):
Administer antipyretics as prescribed.
Consider cold compresses or tepid sponging.
If fever persists after 4 hours, escalate to a healthcare provider for further evaluation.
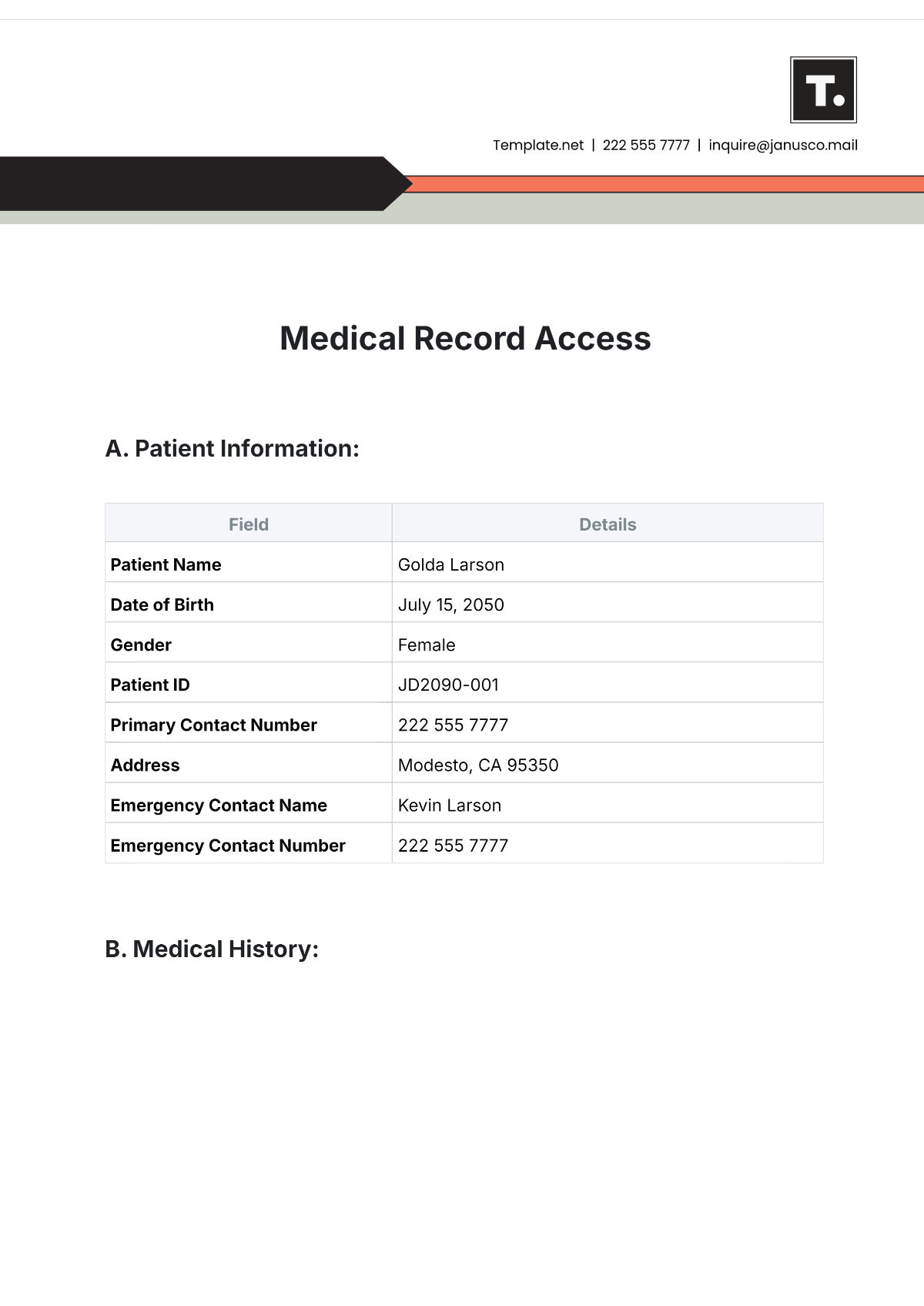
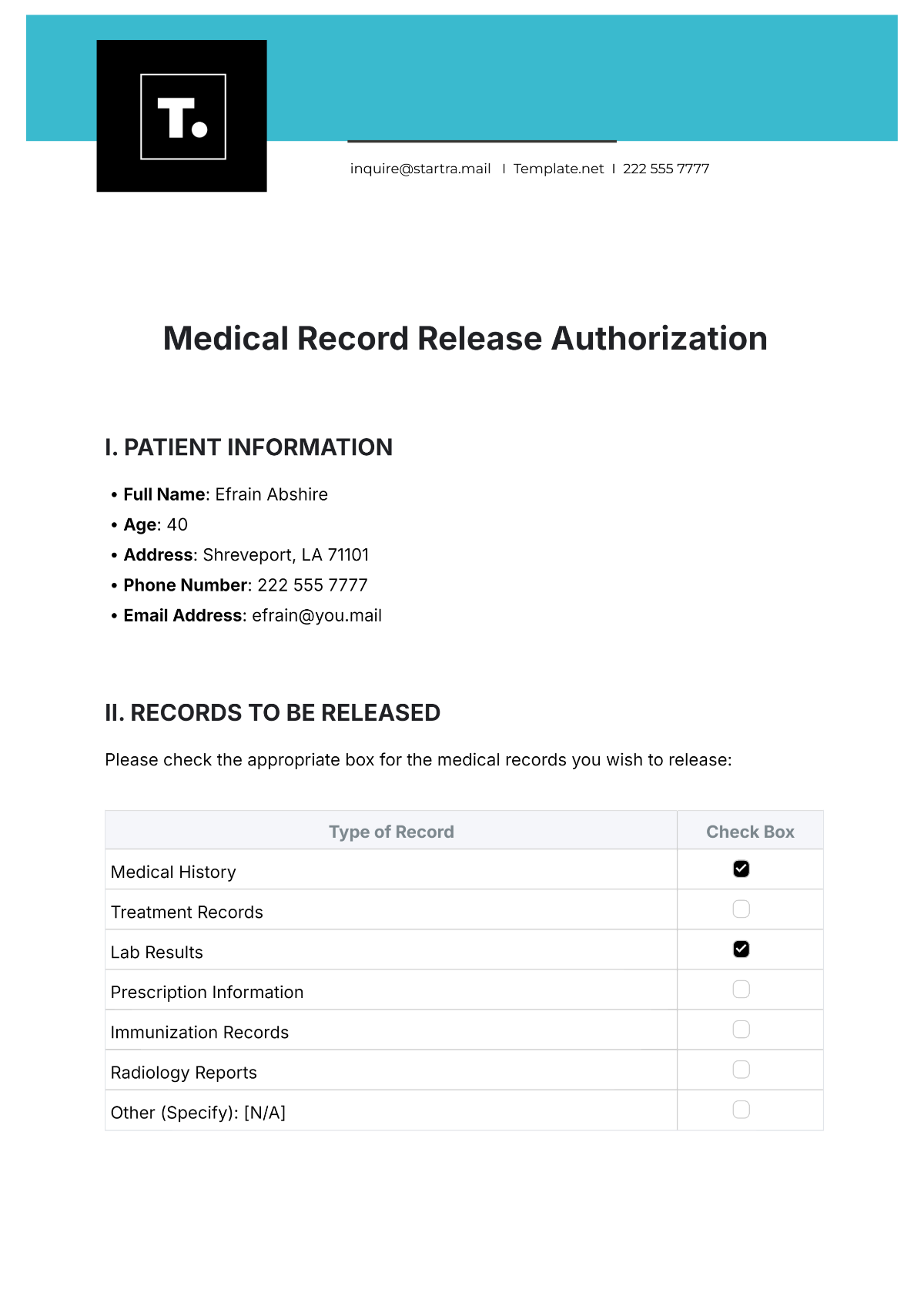
3. Documentation
Record the temperature readings, patient symptoms, and any medications administered in the patient's medical record.
Note the time of re-assessments and any changes in the patient's condition.
4. Follow-Up
If fever persists for more than 48 hours or if the patient’s condition deteriorates, refer to a physician for further evaluation.
Provide the patient with information on when to seek further medical attention (e.g., if new symptoms develop, or if the fever returns after resolution).
References:
World Health Organization (WHO) guidelines on the management of fever.
Institutional policies for the administration of antipyretics.