Nursing Dissertation
Abstract
Evidence-based practice (EBP) integrates the best available research evidence with clinical expertise and patient values to facilitate decision-making and improve healthcare outcomes. This dissertation explores the multifaceted nature of EBP, emphasizing its importance, methodologies, applications, benefits, and challenges within clinical settings. By synthesizing research findings, this study aims to demonstrate how EBP can significantly enhance clinical practice and patient care, ultimately leading to better health outcomes and optimizing resource utilization.
Introduction
The healthcare landscape is continually evolving due to advancements in medical knowledge and technology. Evidence-based practice (EBP) has emerged as a crucial paradigm that prioritizes the use of research findings to refine clinical practice. By combining scientific evidence with clinical expertise and patient preferences, EBP aims to ensure the delivery of optimal healthcare. This dissertation provides an in-depth examination of EBP, exploring its principles, processes, and impact on clinical practice and patient outcomes.
Background
EBP originated in the 2050s as a response to the growing recognition of the gap between research findings and clinical practice. Despite the abundance of scientific research, translating these findings into practical applications within clinical settings proved challenging. EBP was developed to bridge this gap by promoting the use of high-quality evidence in healthcare decision-making and practice.
Significance
The significance of EBP lies in its ability to:
Improve Patient Outcomes: EBP enhances patient safety, quality of care, and overall satisfaction by ensuring that clinical decisions are based on the best available evidence.
Enhance Clinical Efficiency: EBP helps streamline clinical processes, reduce variability in practice, and improve the efficiency of healthcare delivery.
Optimize Resource Utilization: By relying on evidence, healthcare professionals can make informed decisions that lead to more effective use of resources and reduced healthcare costs.
Literature Review
This section reviews the existing literature on EBP, encompassing its definition, frameworks, implementation strategies, and outcomes. The following topics are covered:
Definition and Components of EBP
Frameworks for EBP Implementation
Strategies for Integrating EBP into Clinical Practice
Outcomes of EBP Implementation
Definition and Components of EBP
EBP is defined as the conscientious use of current best evidence in making decisions about patient care. It involves the integration of three fundamental components:
Best Available Evidence: High-quality research findings that are relevant to the clinical context.
Clinical Expertise: The clinician's accumulated experience, education, and clinical skills.
Patient Values and Preferences: The unique preferences, concerns, and expectations of each patient.
Frameworks for EBP Implementation
Various frameworks have been developed to facilitate the implementation of EBP in clinical settings. Notable frameworks include:
Framework | Description |
|---|---|
Model for Evidence-Based Practice Change | A six-step approach involves the identification of clinical issues, evidence review, and evaluation of practice change. |
Johns Hopkins Nursing Evidence-Based Practice Model | A three-phase process focusing on inquiry, practice, and learning to promote EBP. |
PARIHS Framework (Promoting Action on Research Implementation in Health Services) | Emphasizes the interplay between evidence, context, and facilitation in successful EBP implementation. |
Strategies for Integrating EBP into Clinical Practice
Effective integration of EBP into clinical practice requires strategic approaches, including:
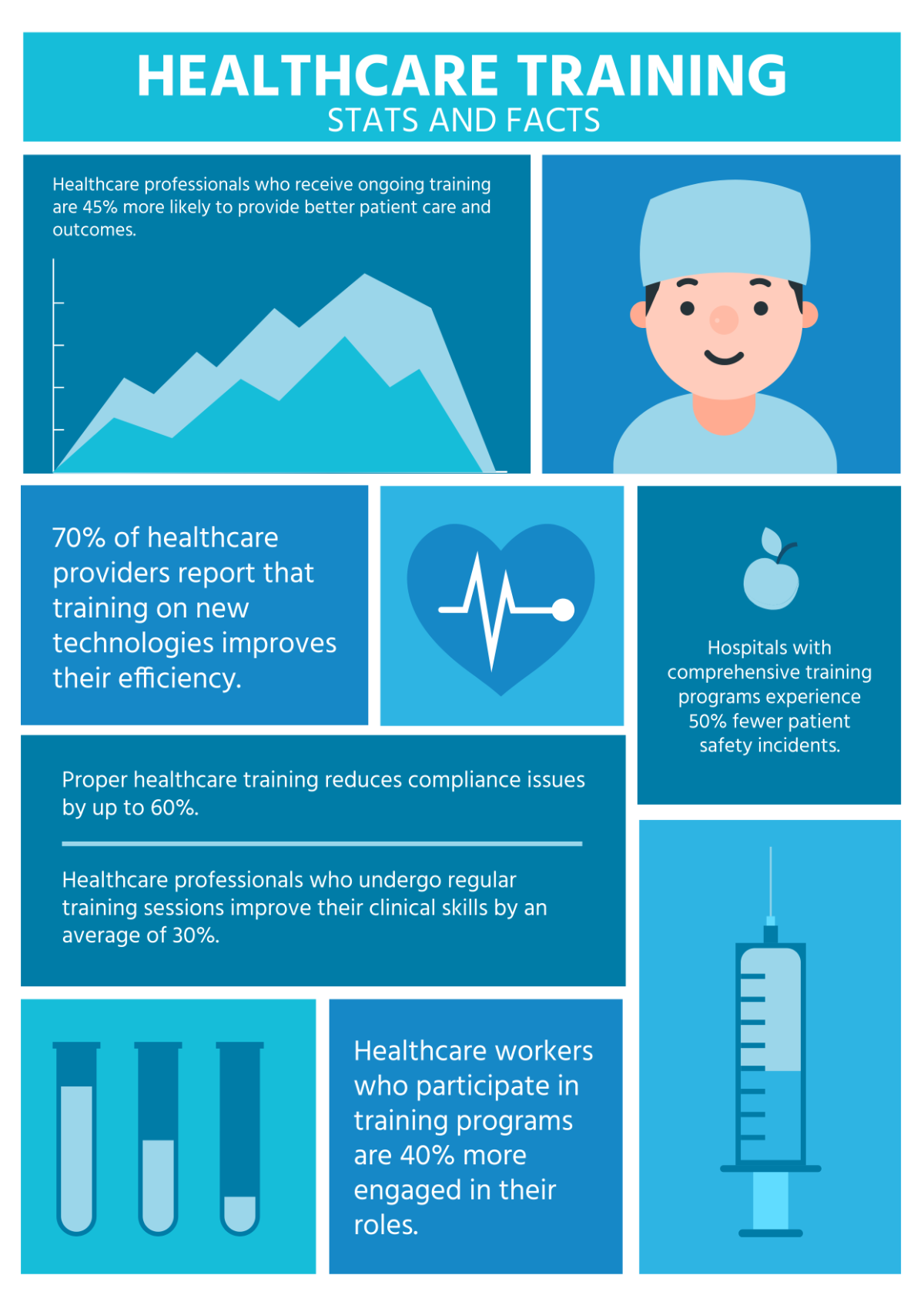
Educational Interventions: Training programs and workshops to enhance clinicians' EBP knowledge and skills.
Mentorship and Collaboration: Support from experienced mentors and interdisciplinary collaboration to foster EBP adoption.
Resources and Tools: Availability of evidence databases, guidelines, and decision support tools.
Organizational Support: Institutional policies and culture that promote and reward EBP activities.
Outcomes of EBP Implementation
EBP implementation has been associated with numerous positive outcomes:
Improved Patient Outcomes: Enhanced patient safety, quality of care, and satisfaction.
Clinical Efficiency: Streamlined processes and reduced practice variation.
Cost-Effectiveness: Efficient use of resources and reduced healthcare costs.
Professional Development: Continued learning and improvement of clinical skills among healthcare professionals.
Methodology
Research Design
A mixed-methods research design was employed, combining quantitative and qualitative approaches to gain comprehensive insights into EBP implementation and outcomes.
Data Collection
Data was collected through the following methods:
Surveys: Structured questionnaires administered to healthcare professionals to assess EBP knowledge, attitudes, and practices.
Interviews: Semi-structured interviews with clinicians and administrators to gather in-depth perspectives on EBP challenges and enablers.
Focus Groups: Group discussions to explore collective experiences and identify common themes.
Document Analysis: Review of institutional policies, guidelines, and EBP training materials.
Data Analysis
Quantitative data from surveys were analyzed using statistical software to identify patterns and correlations. Qualitative data from interviews, focus groups, and document analysis were thematically analyzed to extract meaningful insights and narratives.
Findings
Current State of EBP Implementation
The research revealed varied levels of EBP implementation across different clinical settings. While some institutions demonstrated a strong commitment to EBP, others faced challenges in fully integrating it into practice.
Barriers to EBP Implementation
Several barriers to EBP implementation were identified:
Lack of Time: Clinicians reported insufficient time to appraise and apply research evidence.
Resource Constraints: Limited access to evidence databases and decision support tools.
Knowledge Gaps: Variability in EBP knowledge and skills among healthcare professionals.
Resistance to Change: Reluctance to adopt new practices and alter established routines.
Facilitators of EBP Implementation
Key facilitators that promoted EBP adoption included:
Leadership Support: Strong endorsement of EBP by institutional leaders.
Interdisciplinary Collaboration: Collaborative efforts among clinicians, researchers, and educators.
Continuous Education: Ongoing training and development programs for healthcare professionals.
EHR Integration: Inclusion of evidence-based guidelines and tools in electronic health records (EHRs).
Perceived Outcomes of EBP Implementation
Participants reported several positive outcomes resulting from EBP implementation:
Enhanced Patient Care: Improved clinical decision-making and patient management.
Increased Clinician Confidence: Greater confidence in clinical judgments and interventions.
Professional Satisfaction: Higher job satisfaction due to engagement in EBP activities.
Organizational Improvement: Overall enhancement in the quality and reputation of healthcare institutions.
Discussion
Implications for Clinical Practice
The findings underscore the pivotal role of EBP in advancing clinical practice. By leveraging research evidence, clinicians can make more accurate diagnoses, select appropriate interventions, and monitor patient progress effectively. Institutions should prioritize EBP training and create an environment conducive to ongoing professional development.
Policy Recommendations
Based on the research outcomes, the following policy recommendations are proposed:
Mandate EBP Training: Incorporate EBP education into the curricula of medical and nursing schools.
Support Research Activities: Allocate funding for translational research to bridge the gap between research and practice.
Standardize Guidelines: Develop and disseminate standardized evidence-based clinical guidelines.
Foster Collaboration: Encourage interdisciplinary teamwork and partnerships with academic institutions.
Future Research Directions
Further research is needed to explore the long-term impact of EBP on patient outcomes and healthcare systems. Studies should investigate the efficacy of different EBP implementation strategies and identify best practices for overcoming barriers. Additionally, research should examine the role of technology in facilitating EBP adoption.
Conclusion
Evidence-Based Practice is a transformative approach that has the potential to significantly improve clinical practice and patient care. By integrating research evidence with clinical expertise and patient preferences, EBP offers a systematic framework for making informed healthcare decisions. This dissertation highlights the importance of EBP, identifies challenges and facilitators, and provides actionable recommendations for effective implementation. Embracing EBP is crucial for advancing the quality, efficiency, and sustainability of healthcare delivery.
References
A comprehensive list of references, including research articles, books, guidelines, and other relevant publications, is provided to support the content of this dissertation.