Sample ICU SBAR
Prepared by: [Your Name]
I. Situation
Date: August 27, 2050
Location: [Your Company Address]
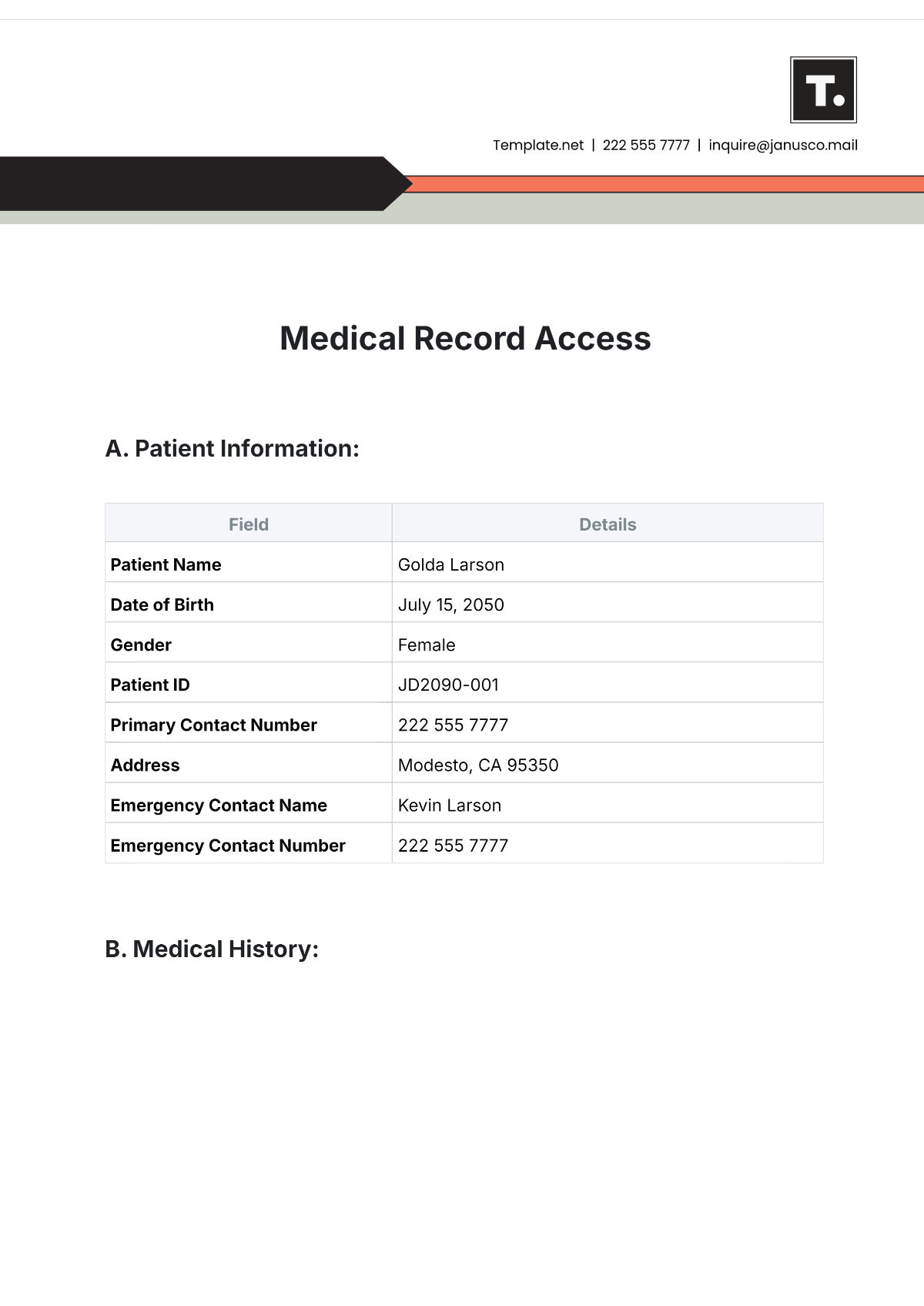
Patient Name: Baby Bartell
Patient ID: 987654
ICU Nurse: [Your Name]
II. Background
Baby Bartell, a 45-year-old female, was admitted to the ICU on August 25, 2050, with acute respiratory distress syndrome (ARDS) following severe pneumonia. She has a history of asthma and recent influenza infection. She is currently on mechanical ventilation and broad-spectrum antibiotics.
Recent Vital Signs:
Vital Sign | Measurement |
|---|---|
Blood Pressure | 92/60 mmHg |
Heart Rate | 98 bpm |
Respiratory Rate | 26 breaths/min |
Temperature | 100.4°F (38°C) |
Current ICU Interventions:
Intervention | Details |
|---|---|
Mechanical Ventilation | Settings: Assist-Control Mode, PEEP 10 cmH2O |
Antibiotics | Meropenem 1g IV q8h |
Sedation | Propofol infusion at 20 mcg/kg/min |
III. Assessment
Baby’s oxygenation is inadequate despite high PEEP settings and increased ventilation support. Her blood pressure remains low, and she shows signs of increasing respiratory distress. There is also evidence of worsening metabolic acidosis on her latest blood gas analysis.
Lab Results:
Test | Result |
|---|---|
Arterial Blood Gas | pH: 7.29, PaCO2: 55 mmHg, HCO3: 22 mEq/L |
Serum Lactate | 4.2 mmol/L |
Creatinine | 1.8 mg/dL |
IV. Recommendation
Immediate Actions:
Increase the tidal volume on the ventilator and reassess ABG results.
Administer a vasopressor (e.g., Epinephrine) to support blood pressure.
Further Monitoring:
Monitor blood gas every 2 hours; adjust ventilator as needed.
Track urine output and electrolytes to guide fluid management.
Consultation:
Consult a pulmonologist about adjusting ventilation.
Request critical care consult for additional therapy evaluation.