SBAR for Sepsis
Prepared by: Dr. [Your Name]
I. Situation
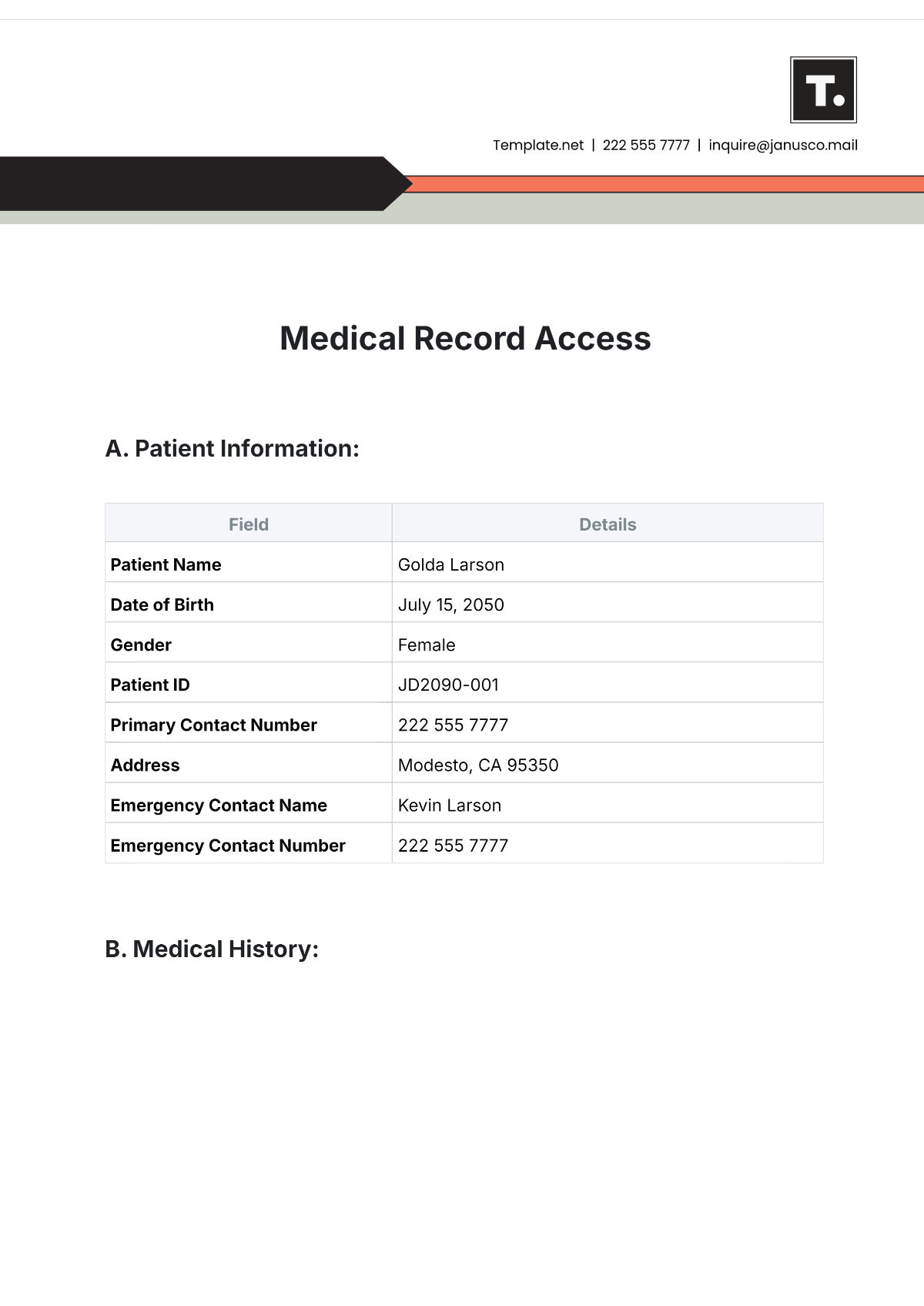
Patient Name: Emily Johnson
Patient ID: 4523-001
Date: August 27, 2050
Emily Johnson is a 68-year-old female presenting with symptoms consistent with sepsis. She was admitted to the emergency department with fever, chills, and rapid breathing. Her initial vital signs showed elevated heart rate and blood pressure irregularities. She has a history of diabetes and chronic kidney disease, which may predispose her to infections.
II. Background
Emily has a medical history notable for diabetes mellitus type 2 and chronic kidney disease. She has recently experienced a urinary tract infection, which was initially managed with antibiotics. However, the symptoms have worsened, and she now presents with increased confusion and decreased urine output. Her current medications include insulin and antihypertensive.
III. Assessment
Based on the clinical presentation and laboratory results, Emily exhibits the following signs of sepsis:
Parameter | Value | Normal Range |
|---|---|---|
Temperature | 102.4°F (39.1°C) | 97.8°F to 99.1°F (36.5°C to 37.3°C) |
Heart Rate | 112 bpm | 60-100 bpm |
Respiratory Rate | 24 breaths/min | 12-20 breaths/min |
Blood Pressure | 88/56 mmHg | 90/60 to 120/80 mmHg |
White Blood Cell Count | 18,000/µL | 4,000-11,000/µL |
Lactate Level | 3.2 mmol/L | 0.5-2.2 mmol/L |
Emily's clinical status indicates a severe systemic infection. The high lactate level and elevated white blood cell count suggest a significant inflammatory response. Her decreased urine output and altered mental status further support the diagnosis of sepsis.
IV. Recommendation
Immediate intervention is required to manage sepsis effectively:
Antibiotic Therapy: Initiate broad-spectrum antibiotics as per sepsis protocol. Suggested antibiotics include Piperacillin-Tazobactam or Meropenem pending further culture results.
Fluid Resuscitation: Administer intravenous fluids to maintain blood pressure and support renal function. Start with crystalloids, such as Normal Saline, at a rate of 30 mL/kg.
Vasopressor Support: Consider norepinephrine infusion if hypotension persists despite adequate fluid resuscitation.
Monitoring: Continuous monitoring of vital signs, urine output, and lactate levels. Perform frequent blood gas analyses and adjust treatment as necessary.
Consultations: Immediate consultation with an infectious disease specialist and nephrologist for further management.