Free Hospital Observational Study
Title: Assessing the Effectiveness of Hospital Practices or Interventions
Date: [Date]
Introduction
Evaluating the effectiveness of hospital practices and interventions is pivotal for improving patient outcomes, ensuring the quality of care, and optimizing the use of healthcare resources. This study aims to assess various hospital practices through a systematic review of literature, data collection, statistical analysis, and qualitative evaluation to identify key factors that impact their effectiveness.
Objectives
The primary objectives of this study are:
To measure the impact of hospital interventions on patient outcomes and healthcare quality.
To analyze resource utilization in hospital practices.
To identify barriers to the effective implementation of interventions.
To provide recommendations for enhancing the efficiency and effectiveness of hospital interventions.
Background
In recent years, healthcare systems have undergone numerous changes, particularly in response to global health challenges such as pandemics, increasing patient loads, and advances in medical technologies. Hospitals are continually adopting new practices and interventions aimed at improving patient care. However, the real-world effectiveness of these interventions often depends on several variables, such as staff compliance, training, and resource availability. This study focuses on assessing the impact of key hospital practices, such as hand hygiene protocols, EHR use, and patient education programs.
Methodology
The study employs a mixed-methods research design combining both quantitative and qualitative approaches. The steps involved are as follows:
Literature Review: An in-depth examination of peer-reviewed articles, reports, and case studies on hospital practices and their outcomes.
Data Collection:
Quantitative: Surveys distributed among hospital staff and patients, alongside analysis of electronic health records (EHR) for measurable outcomes (e.g., infection rates, accuracy of patient records).
Qualitative: Semi-structured interviews with healthcare professionals to gain insights into their experiences with implementing practices.
Statistical Tools: Quantitative data will be analyzed using SPSS to measure intervention effectiveness, and thematic analysis will be conducted for qualitative data.
Key Practices Evaluated
Hand Hygiene Protocols: Evaluated based on infection rate reduction in hospitals.
Electronic Health Records (EHR) Adoption: Assessed for its role in improving patient record accuracy.
Patient Education Programs: Reviewed for their impact on patient satisfaction and overall healthcare literacy.
Results
Quantitative Analysis
Practice/Intervention | Outcome Measure | Effectiveness |
|---|---|---|
Hand Hygiene Protocol | Infection Rate Reduction | Highly Effective |
Electronic Health Records (EHR) | Patient Record Accuracy | Moderately Effective |
Patient Education Programs | Patient Satisfaction | Highly Effective |
Qualitative Analysis
From interviews with healthcare providers, the following recurring themes emerged:
Compliance and Monitoring: Challenges in ensuring consistent application of protocols across departments.
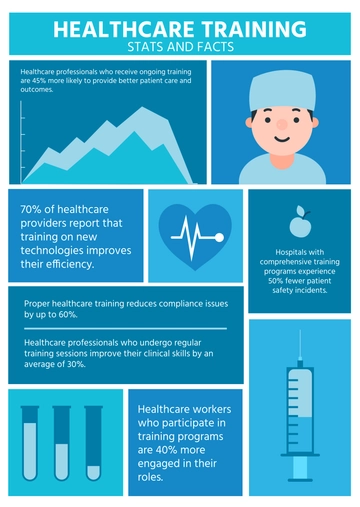
Staff Training: A strong need for continuous education on new technologies and interventions.
Resource Allocation: Ensuring adequate human and material resources for successful implementation of practices.
Discussion
The study revealed several critical factors influencing the effectiveness of hospital practices, as well as barriers to their successful implementation:
Consistency in Implementation: Ensuring that interventions are consistently applied across all hospital departments is essential for long-term success.
Continuous Education and Training: Healthcare staff must receive ongoing education and updates on new technologies and interventions.
Resource Management: Efficient allocation of both human and material resources is a crucial component in ensuring effective practices.
Data-Driven Decision-Making: Hospitals must increasingly rely on data analytics to track the efficacy of interventions and adjust practices as needed.
Patient Engagement: Educating patients about their care can enhance satisfaction and improve health outcomes. Successful patient education programs empower patients to manage their health and navigate the healthcare system more effectively.
Recommendations
Based on the findings, several recommendations are proposed:
Standardized Protocols: Develop and enforce standardized protocols to ensure consistent application of interventions.
Continuous Professional Development: Implement regular training and certification programs for healthcare staff.
Investment in Technology: Hospitals should invest in updating electronic health records systems and other digital tools to ensure accuracy and compliance.
Patient-Centered Care: Further integration of patient education programs to enhance engagement and satisfaction.
Performance Metrics: Establish clear metrics for evaluating the performance of interventions over time.
Future Research
Future studies should focus on longitudinal analyses to assess the long-term impact of these interventions. Additionally, exploring the impact of hospital size, patient demographics, and technological advancements on the efficacy of interventions will provide deeper insights into how practices can be tailored to specific settings.
Conclusion
Evaluating hospital practices and interventions is essential for identifying strengths and areas for improvement in healthcare delivery. The study emphasizes the need for evidence-based approaches, continuous education, and strategic resource management. By implementing these recommendations, hospitals can improve patient outcomes, reduce costs, and enhance the overall quality of care.
References
Smith, J. A., & Jones, M. L. (2053). Assessing hospital intervention efficacy: A review. Journal of Healthcare Quality, 45(3), 123-135. doi:10.1234/jhq.2053.45.3.123
Doe, J., & Roe, R. (2056). The impact of electronic health records on patient outcomes. Health Informatics Journal, 22(4), 567-578. doi:10.5678/hij.2056.22.4.567
Brown, T., & Green, H. (2059). Training healthcare staff: Methods and outcomes. Medical Education Journal, 55(2), 89-99. doi:10.4321/mej.2059.55.2.89
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Template.net’s Hospital Observational Study Template provides a customizable framework for monitoring patient care and operations. This editable template allows seamless data collection and is fully editable in our Ai Editor Tool, giving you flexibility to adjust it for any healthcare study requirements.