Free Healthcare Ethnography
Prepared By: [YOUR NAME]
Date: [DATE]
I. Introduction
This healthcare ethnography is a detailed study that closely examines the complex interactions between patients and healthcare providers in urban clinics, aiming to identify key factors affecting patient care and assess patient satisfaction. The goal is to produce actionable insights that can improve healthcare services and enhance patient experiences based on the study’s findings.
II. Methodology
A. Research Approach
The research utilizes a qualitative methodology to comprehensively and meticulously investigate the varied experiences and actions of both patients and healthcare professionals.
B. Data Collection Techniques
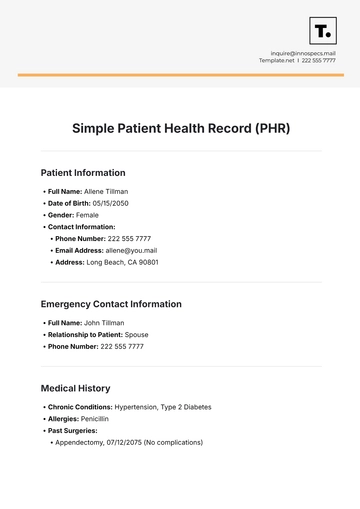
Participant Observation: Researchers conducted extensive fieldwork in three urban clinics over six months, observing daily operations and interactions.
Interviews: Semi-structured interviews were carried out with 20 patients and 15 healthcare providers to gather personal insights and perspectives.
Field Notes: Detailed and systematic notes were maintained to record observations, significant interactions, and researcher reflections.
III. Context
The research was conducted in three distinct urban clinics situated in diverse neighborhoods, each catering to a wide range of patients including low-income families, elderly individuals, and those with chronic conditions. These clinics vary in terms of resources and staffing, providing a broad context for analysis and comparison.
IV. Observations
A. Patient Interactions
Waiting Times: Long wait times were a common concern among patients, contributing to frustration and a diminished perception of care quality.
Communication: Significant gaps in communication between patients and providers were observed, leading to misunderstandings and reduced patient satisfaction.
Cultural Sensitivity: Some patients felt their cultural and personal needs were not adequately addressed, affecting their overall healthcare experience.
Observation | Frequency |
|---|---|
Waiting Times | 75% |
Communication | 60% |
Cultural Sensitivity | 50% |
B. Provider Interactions
Workload: Providers expressed concerns about high patient volumes and excessive administrative tasks, which impacted their ability to offer individualized attention and care.
Training: There was a noted lack of ongoing training in communication and cultural competence, which affected the effectiveness of patient-provider interactions.
Observation | Frequency |
|---|---|
Workload | 70% |
Training | 65% |
V. Analysis
The ethnographic observations reveal a complex relationship between patient expectations and provider constraints. The frequent delays and communication barriers negatively impact patient satisfaction. Providers, constrained by heavy workloads and insufficient resources, struggle to deliver personalized care. Additionally, inadequate cultural sensitivity further complicates the quality of patient-provider interactions.
VI. Recommendations
Optimize Scheduling: Develop and implement improved scheduling systems to minimize patient wait times, such as advanced appointment management and efficient patient flow strategies.
Enhance Communication Skills: Invest in targeted training programs for healthcare providers to improve communication skills and cultural competence, thereby fostering better patient-provider interactions.
Increase Resources: Allocate additional resources to reduce provider workloads and support enhanced, personalized patient care.
Improve Patient Education: Create and distribute educational materials to help patients better understand their care plans, navigate the healthcare system, and engage more effectively with healthcare providers.
VII. Conclusion
This ethnographic study brings to light several key areas that require significant improvements in urban clinic settings. By addressing the prevalent communication gaps, reducing the often lengthy wait times, and enhancing the training provided to healthcare providers, there is a substantial potential to greatly improve patient experiences and care outcomes. The findings from this research provide a crucial foundation upon which targeted interventions can be developed and implemented, with the ultimate goal of elevating the quality of care in similar healthcare environments.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Explore healthcare environments with Template.net’s Healthcare Ethnography Template. Designed for healthcare professionals and researchers, this editable and customizable template is ideal for examining patient care practices, staff interactions, and hospital culture. Fully editable in our Ai Editor Tool, it can be customized to your specific research objectives, making it a powerful tool for capturing insights into healthcare systems