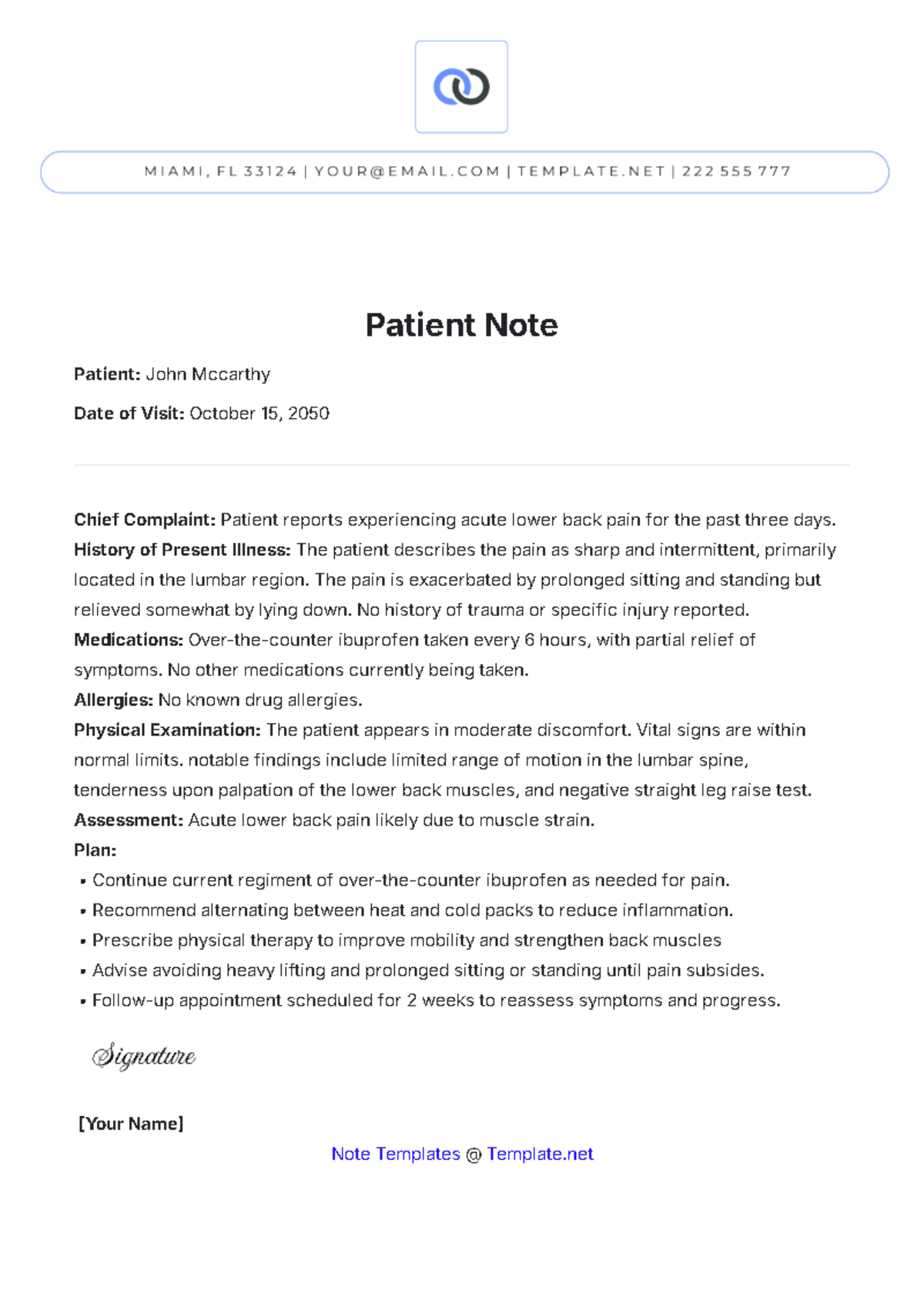
Patient Note
Patient: John Mccarthy
Date of Visit: October 15, 2050
Chief Complaint: Patient reports experiencing acute lower back pain for the past three days.
History of Present Illness: The patient describes the pain as sharp and intermittent, primarily located in the lumbar region. The pain is exacerbated by prolonged sitting and standing but relieved somewhat by lying down. No history of trauma or specific injury reported.
Medications: Over-the-counter ibuprofen taken every 6 hours, with partial relief of symptoms. No other medications currently being taken.
Allergies: No known drug allergies.
Physical Examination: The patient appears in moderate discomfort. Vital signs are within normal limits. notable findings include limited range of motion in the lumbar spine, tenderness upon palpation of the lower back muscles, and negative straight leg raise test.
Assessment: Acute lower back pain likely due to muscle strain.
Plan:
Continue current regiment of over-the-counter ibuprofen as needed for pain.
Recommend alternating between heat and cold packs to reduce inflammation.
Prescribe physical therapy to improve mobility and strengthen back muscles
Advise avoiding heavy lifting and prolonged sitting or standing until pain subsides.
Follow-up appointment scheduled for 2 weeks to reassess symptoms and progress.

[Your Name]
Note Templates @ Template.net