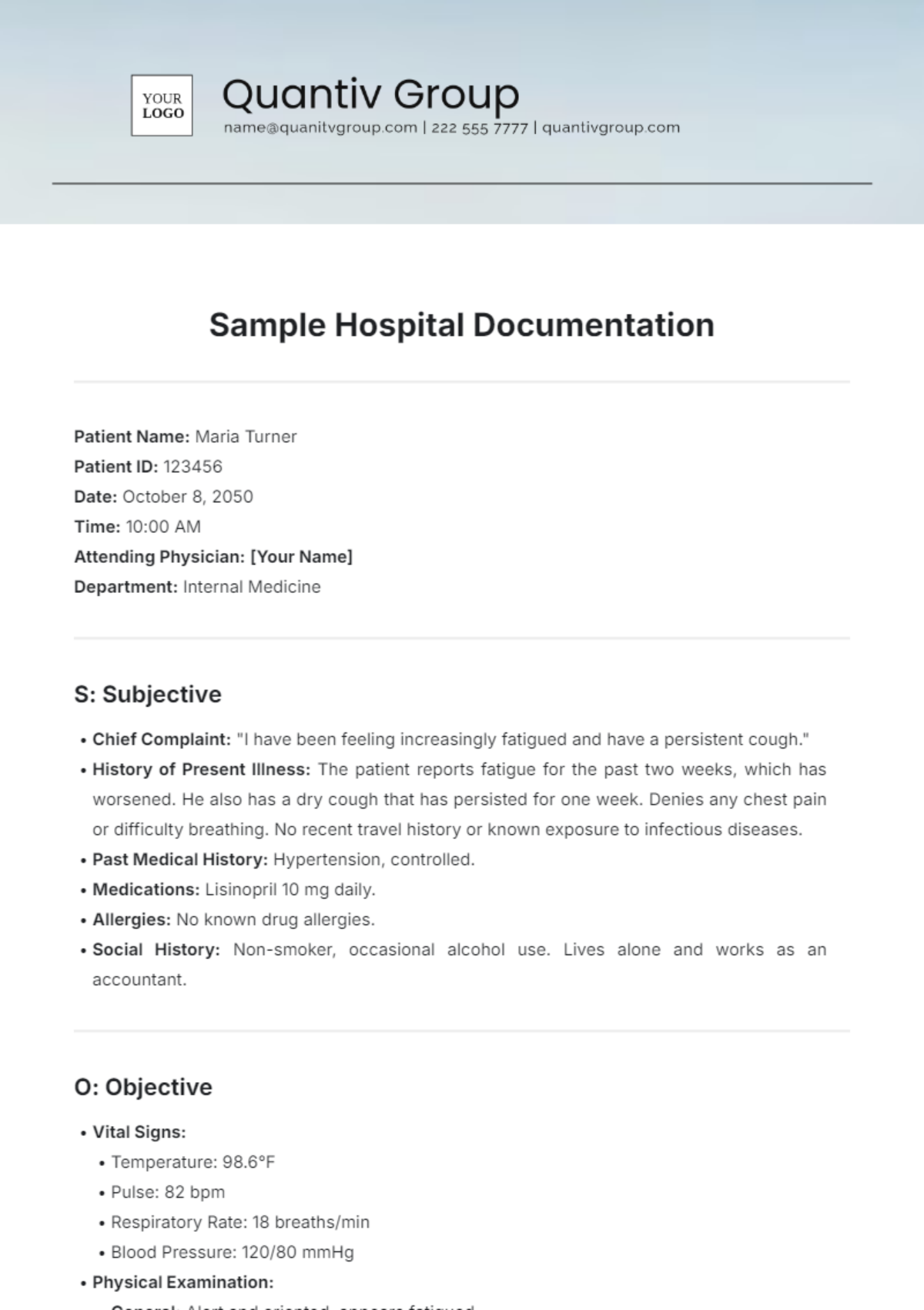
Sample Hospital Documentation
Patient Name: Maria Turner
Patient ID: 123456
Date: October 8, 2050
Time: 10:00 AM
Attending Physician: [Your Name]
Department: Internal Medicine
S: Subjective
Chief Complaint: "I have been feeling increasingly fatigued and have a persistent cough."
History of Present Illness: The patient reports fatigue for the past two weeks, which has worsened. He also has a dry cough that has persisted for one week. Denies any chest pain or difficulty breathing. No recent travel history or known exposure to infectious diseases.
Past Medical History: Hypertension, controlled.
Medications: Lisinopril 10 mg daily.
Allergies: No known drug allergies.
Social History: Non-smoker, occasional alcohol use. Lives alone and works as an accountant.
O: Objective
Vital Signs:
Temperature: 98.6°F
Pulse: 82 bpm
Respiratory Rate: 18 breaths/min
Blood Pressure: 120/80 mmHg
Physical Examination:
General: Alert and oriented, appears fatigued.
Respiratory: Clear to auscultation bilaterally, no wheezes or crackles.
Cardiovascular: Regular rate and rhythm, no murmurs.
Abdomen: Soft, non-tender, no organomegaly.
Laboratory Results:
CBC: Mild leukocytosis
Chest X-ray: No acute infiltrates or effusions
A: Assessment
Fatigue, likely related to viral illness (rule out COVID-19).
Persistent cough, likely due to post-viral irritation.
Hypertension is well-controlled.
P: Plan
Labs: Order COVID-19 PCR test.
Medications: Recommend over-the-counter cough suppressants as needed.
Follow-up: Schedule a follow-up appointment in one week or sooner if symptoms worsen.
Education: Educate the patient on hydration, rest, and monitoring symptoms. Advise to seek immediate care if difficulty breathing or chest pain occurs.
Signature:

[Your Name]
Date: October 8, 2050