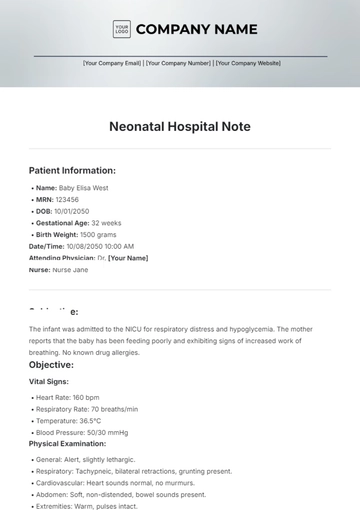
Free Neonatal Hospital Note
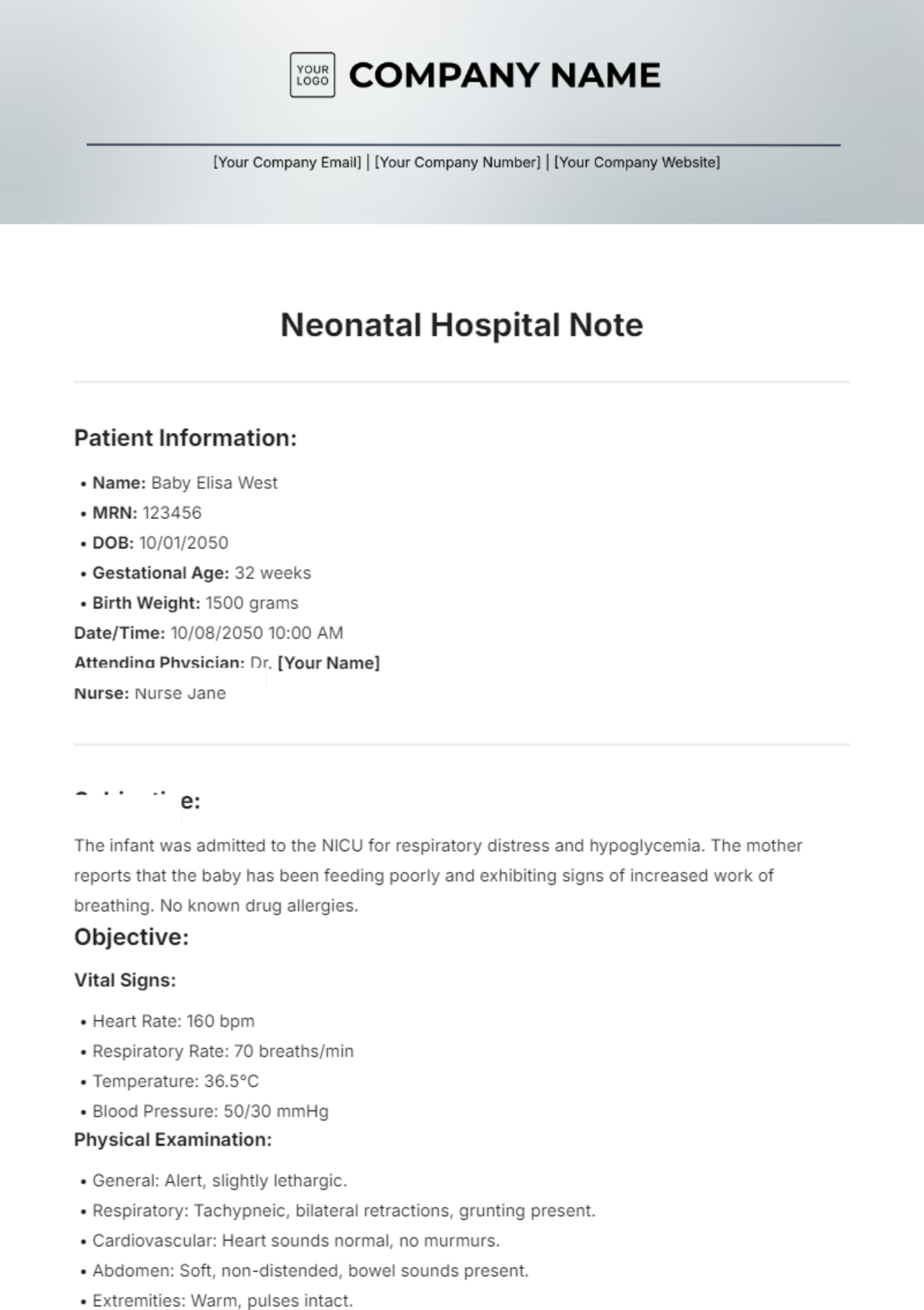
Patient Information:
Name: Baby Elisa West
MRN: 123456
DOB: 10/01/2050
Gestational Age: 32 weeks
Birth Weight: 1500 grams
Date/Time: 10/08/2050 10:00 AM
Attending Physician: Dr. [Your Name]
Nurse: Nurse Jane
Subjective:
The infant was admitted to the NICU for respiratory distress and hypoglycemia. The mother reports that the baby has been feeding poorly and exhibiting signs of increased work of breathing. No known drug allergies.
Objective:
Vital Signs:
Heart Rate: 160 bpm
Respiratory Rate: 70 breaths/min
Temperature: 36.5°C
Blood Pressure: 50/30 mmHg
Physical Examination:
General: Alert, slightly lethargic.
Respiratory: Tachypneic, bilateral retractions, grunting present.
Cardiovascular: Heart sounds normal, no murmurs.
Abdomen: Soft, non-distended, bowel sounds present.
Extremities: Warm, pulses intact.
Laboratory Results:
CBC: Hemoglobin 12 g/dL, WBC 10,000/µL, Platelets 150,000/µL
Blood Glucose: 40 mg/dL (given D10W bolus)
ABG: pH 7.35, pCO2 55 mmHg, pO2 60 mmHg
Assessment:
Preterm infant (32 weeks) with respiratory distress likely secondary to immature lung development and possible hypoglycemia.
Requires ongoing monitoring and supportive care.
Plan:
Continue oxygen therapy via nasal cannula.
Monitor vital signs every 2 hours.
Initiate enteral feeds with fortified breast milk, starting at 10 mL/kg/day.
Repeat blood glucose monitoring every 6 hours.
Consult neonatology for further evaluation of respiratory distress and potential CPAP initiation.
Parent education regarding signs of respiratory distress and feeding.
Signature:

Dr. [Your Name], MD
Neonatologist
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Introducing the Neonatal Hospital Note Template from Template.net! This fully customizable and editable template is designed for healthcare professionals. Easily modify patient information and medical details using our AI Editor Tool, ensuring accuracy and efficiency in documentation. Streamline your workflow and enhance patient care with this essential resource tailored for neonatal care.
You may also like
- Delivery Note
- Notes Release
- Concept Note
- Class Note
- Hospital Note
- Apology Note
- Credit Note
- Handover Note
- Personal Note
- Excuse Note
- Case Note
- Sample Doctor Note
- Lesson Note
- Appointment Note
- Piano Note
- School Note
- Progress Note
- Business Note
- SOAP Note Templates
- Therapy Note
- Briefing Note
- Summary Note
- Sample Note
- Printable Note