Soap Notes
Prepared by: [Your Name]
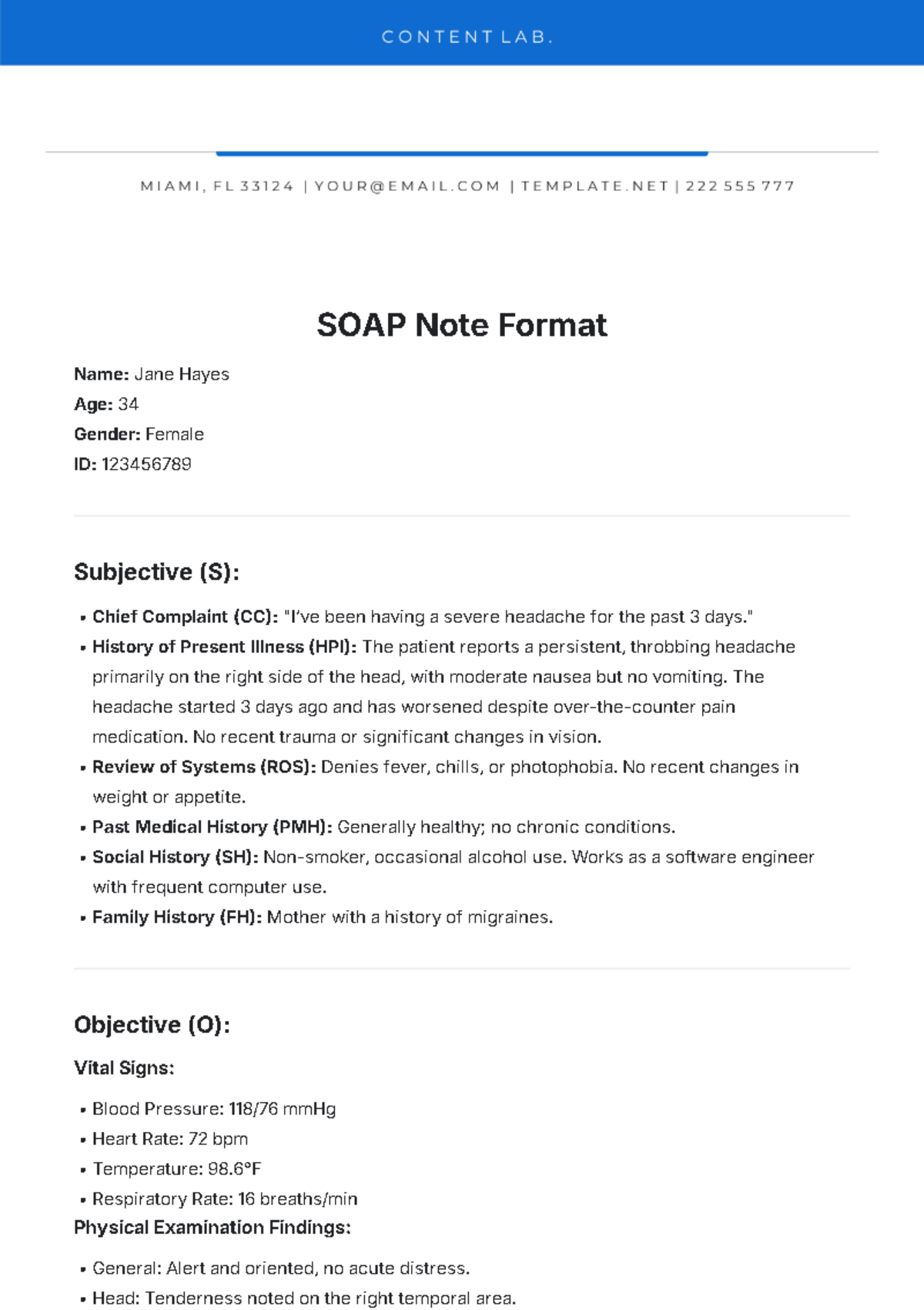
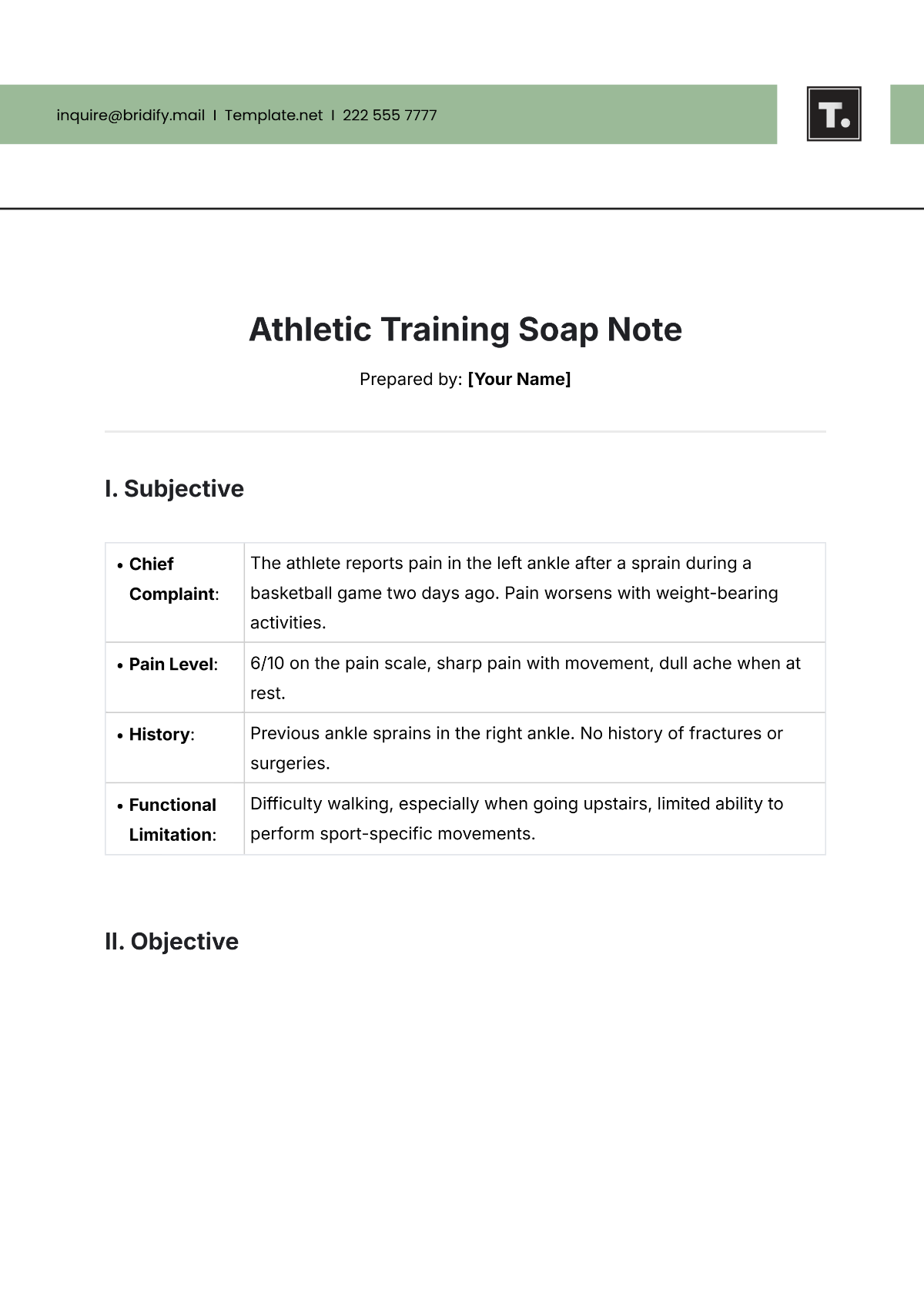
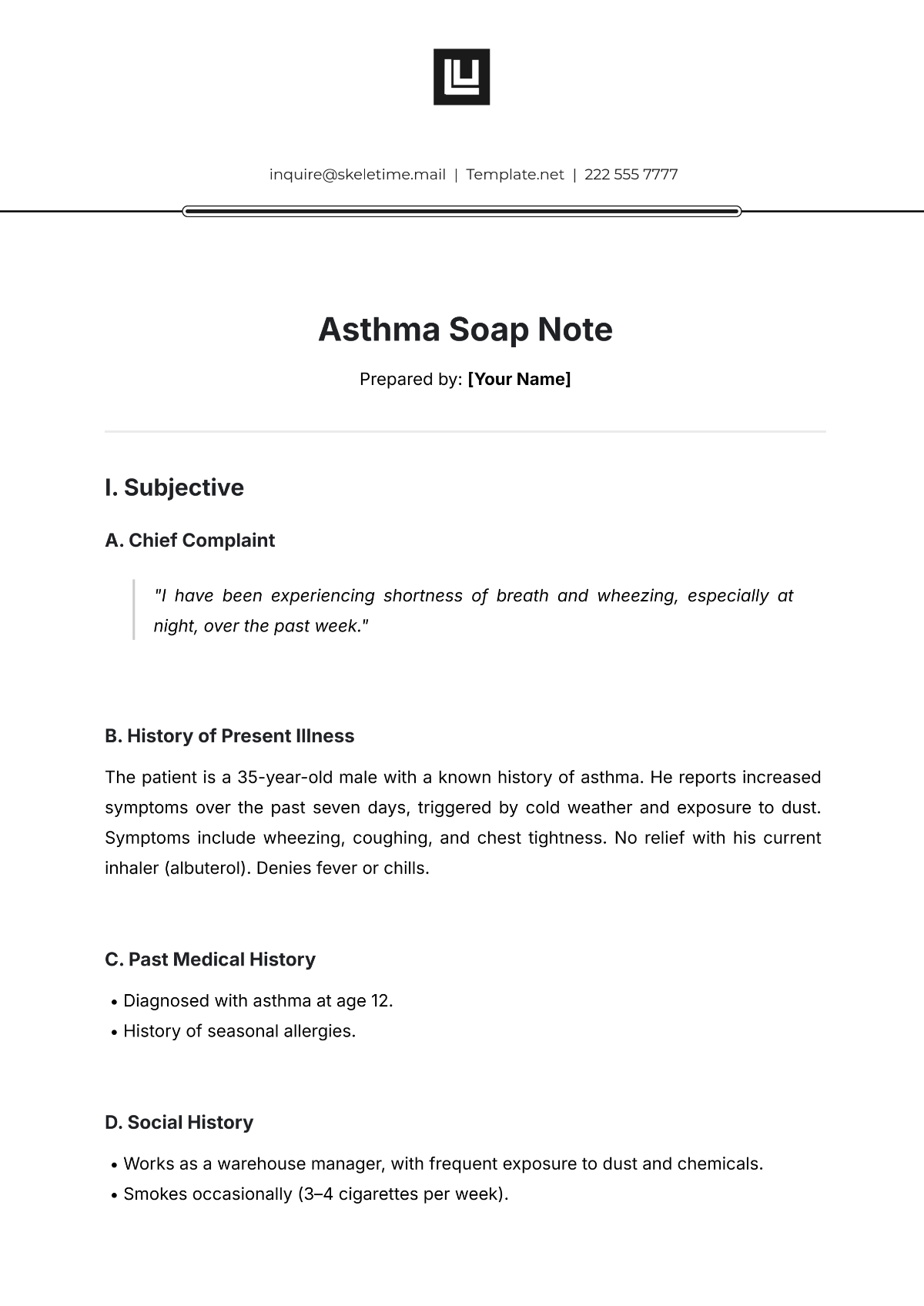
I. Subjective (S)
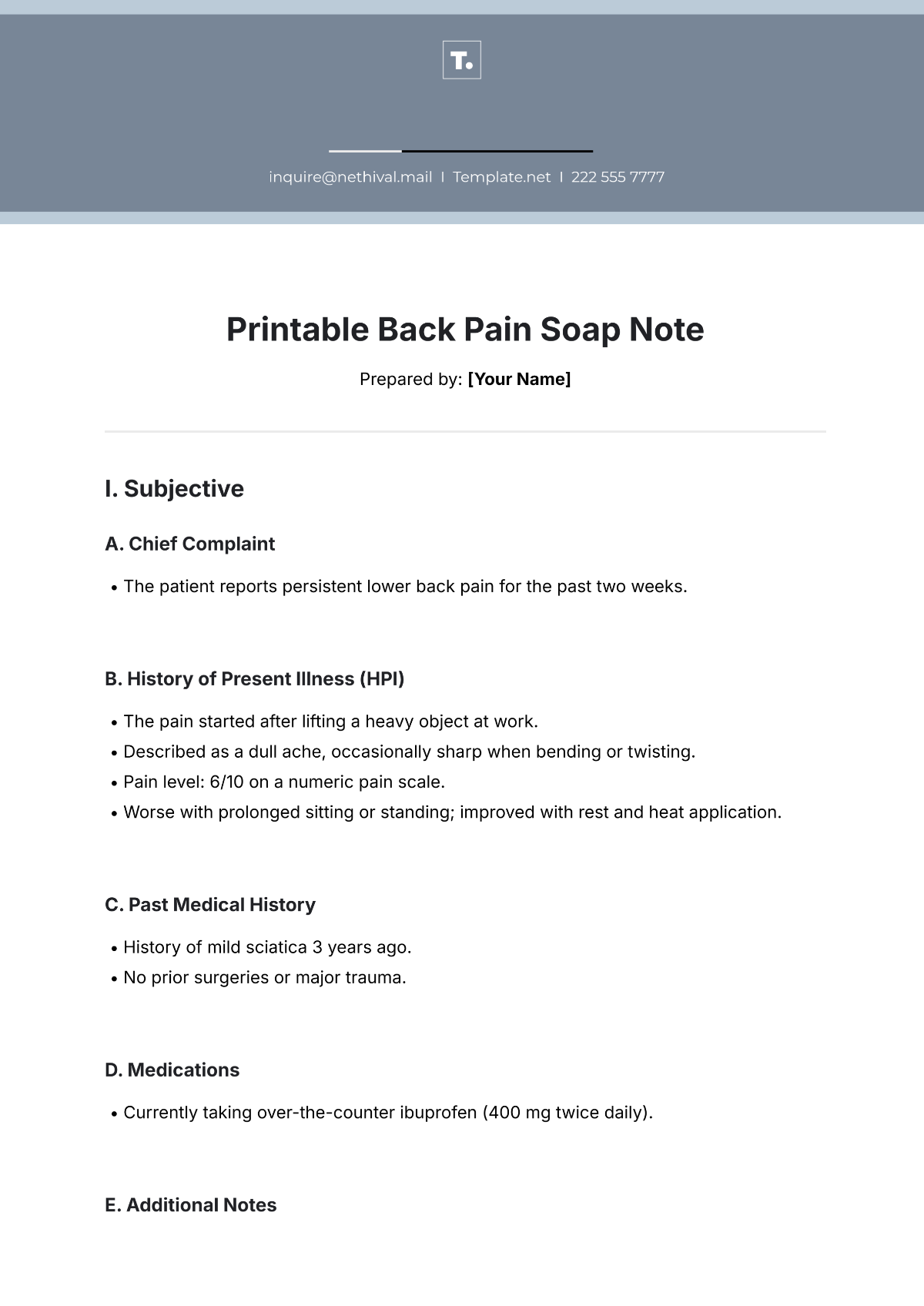
A. Chief Complaint (CC)
"I have been experiencing persistent back pain for the last week."
B. History of Present Illness (HPI)
The patient reports dull, aching lower back pain, which started gradually and has worsened over the past 5 days. The pain is constant, rated 6/10 on the pain scale, and is aggravated by prolonged sitting and bending. The patient notes no relief from over-the-counter pain medications.
C. Review of Systems (ROS)
System | Findings |
|---|---|
Musculoskeletal | Positive for lower back pain. |
Neurological | No numbness or tingling in the legs. |
Gastrointestinal | Denies nausea, vomiting, or changes in bowel movements. |
D. Past Medical History (PMH)
No history of chronic back issues. No previous surgeries.
E. Medications
Over-the-counter ibuprofen for pain.
II. Objective (O)
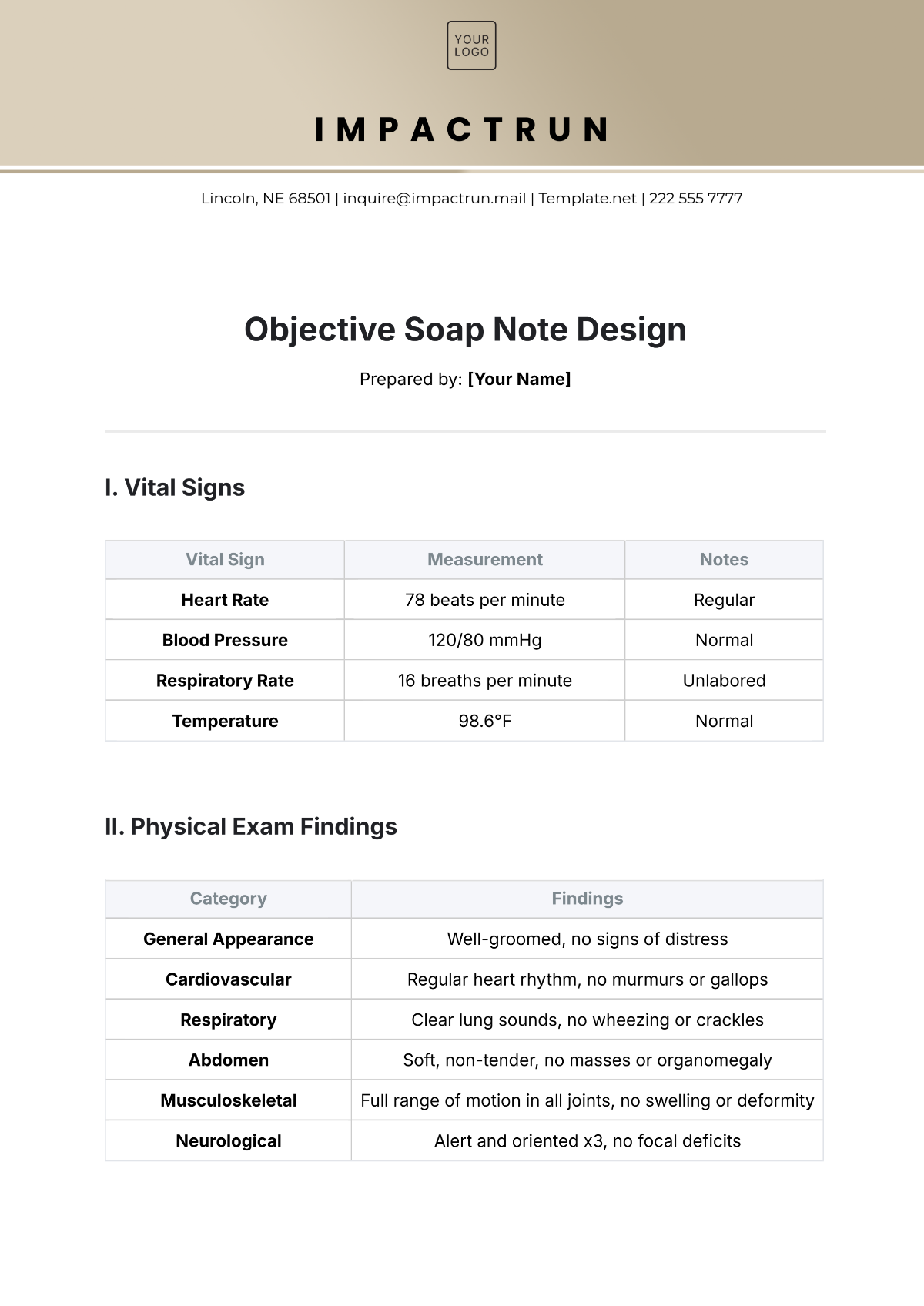
A. Vital Signs
Vital Sign | Measurement |
|---|---|
Blood Pressure | 120/78 mmHg |
Heart Rate | 78 bpm |
Temperature | 98.6°F |
Respiratory Rate | 16 breaths/min |
B. Physical Exam:
Exam Type | Findings |
|---|---|
Inspection | No visible deformities or swelling in the back. |
Palpation | Tenderness was noted over the lumbar spine, particularly at L4-L5. |
Range of Motion (ROM) | Reduced lumbar flexion due to pain. |
Neurological | Normal reflexes, sensation, and motor function in both legs. |
C. Diagnostic Tests
No imaging was done at this point. Consideration for an X-ray or MRI if symptoms persist.
III. Assessment (A)
A. Primary Diagnosis
Acute lower back pain, likely muscular strain.
B. Differential Diagnosis
Lumbar disc herniation
Spinal stenosis
C. Clinical Interpretation
The patient's symptoms suggest a muscular strain in the lumbar region. No signs of neurological impairment or red flags for more serious conditions.
IV. Plan (P)
A. Treatment Plan
Continue ibuprofen for pain relief.
Recommend heat therapy and gentle stretching exercises to improve mobility.
Encourage proper posture while sitting and standing.
B. Referrals
If pain persists beyond 2 weeks or worsens, consider referral to physical therapy or orthopedic specialist for further evaluation.
C. Follow-up
Follow up in 1 week for re-assessment of symptoms.