Free Pharmacology Case Study
1. Introduction
This case study aims to analyze a clinical scenario from a pharmacological perspective, evaluating the patient details, diagnosis, treatment plans, and outcomes. This template is designed for healthcare professionals to systematically study and present cases to enhance clinical learning and improve patient care.
2. Case Overview
Patient Profile
Attribute | Details |
|---|---|
Name | John Doe |
Age | 54 |
Gender | Male |
Medical History | Hypertension, Type 2 Diabetes |
A. Chief Compliant
The patient presented with chest pain and shortness of breath, which have been persistent for the last two days.
B. Clinical Presentation
Vital Signs: BP 150/95 mmHg, HR 88 bpm, RR 20 breaths/min, Temp 37.6°C
Physical Examination: Elevated jugular venous pressure, bilateral lung crackles
Diagnostic Tests: ECG showing ST-elevation, Elevated Troponin levels
3. Diagnosis
The patient is diagnosed with acute myocardial infarction (MI), commonly referred to as a heart attack, based on the presenting symptoms, physical examination, and diagnostic test results.
4. Pharmacological Management
A. Initial Treatment Plan
Upon diagnosis, the immediate goal is to restore coronary blood flow, manage symptoms, and prevent further complications. The initial pharmacological therapy includes:
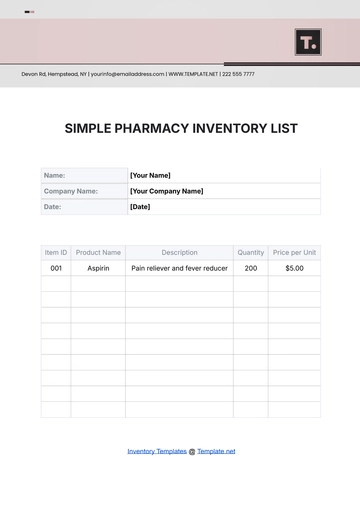
Aspirin 325 mg orally, to inhibit platelet aggregation
Nitroglycerin sublingually, to relieve chest pain
Clopidogrel 300 mg orally, as a secondary antiplatelet agent
Statins to control cholesterol level
Beta-blockers to reduce myocardial oxygen demand
B. Ongoing Management
Following the initial treatment, the ongoing management focuses on secondary prevention and lifestyle modifications. The pharmacological therapy includes:
ACE inhibitors such as Ramipril 5 mg once daily
SGLT2 inhibitors for glycemic control in diabetes
Low dose Aspirin 75 mg daily as maintenance
Continuous Statin therapy like Atorvastatin 40 mg daily
5. Patient Monitoring
Regular monitoring of the patient's condition and response to the treatment is crucial for optimizing outcomes. Key monitoring parameters include:
Electrocardiogram (ECG) to assess heart rhythm and ischemic changes
Blood pressure monitoring to ensure controlled blood pressure
Lipid profile every 3 months
Routine blood glucose tests for diabetes management
6. Outcomes and Discussions
A. Clinical Outcome
After two weeks of treatment, the patient's condition improved significantly. The chest pain subsided, and follow-up ECGs showed no further ST elevation. Troponin levels returned to normal ranges.
B. Factors Influencing Outcomes
Several factors contributed to the patient's positive outcome, including timely intervention, adherence to medication, and lifestyle modifications such as dietary changes and smoking cessation.
C. Potential Challenges
Challenges such as adherence to medication regimen and side effects of medications (e.g., persistent cough from ACE inhibitors) need to be addressed through patient education and personalized care plans.
7. Conclusion
This case study illustrates the importance of comprehensive pharmacological management in acute myocardial infarction cases. Through effective treatment plans and monitoring, patients can achieve significant recovery and prevent future cardiovascular events. Continued research and education are vital to advancing pharmacological practices and improving patient care.
References
A list of references to relevant clinical guidelines, studies, and textbooks that were consulted in the preparation of this case study.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Template.net’s Pharmacology Case Study Template provides a clear, structured approach to documenting pharmacological studies. Customizable and fully editable, this template ensures your reports are tailored to your research needs. Editable in our Ai Editor Tool, it allows you to make adjustments with ease, providing a seamless way to present detailed pharmacology case studies effectively.