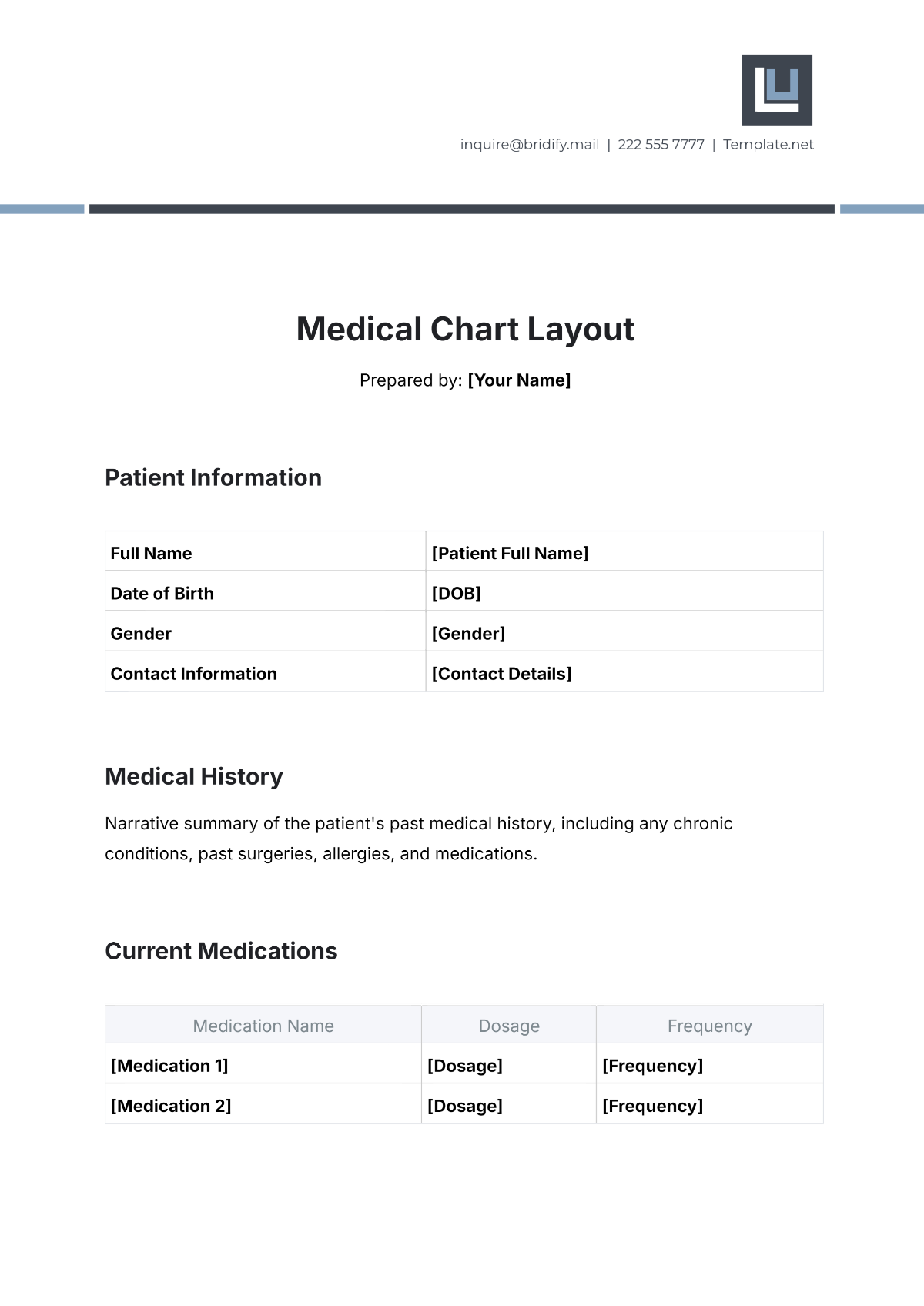
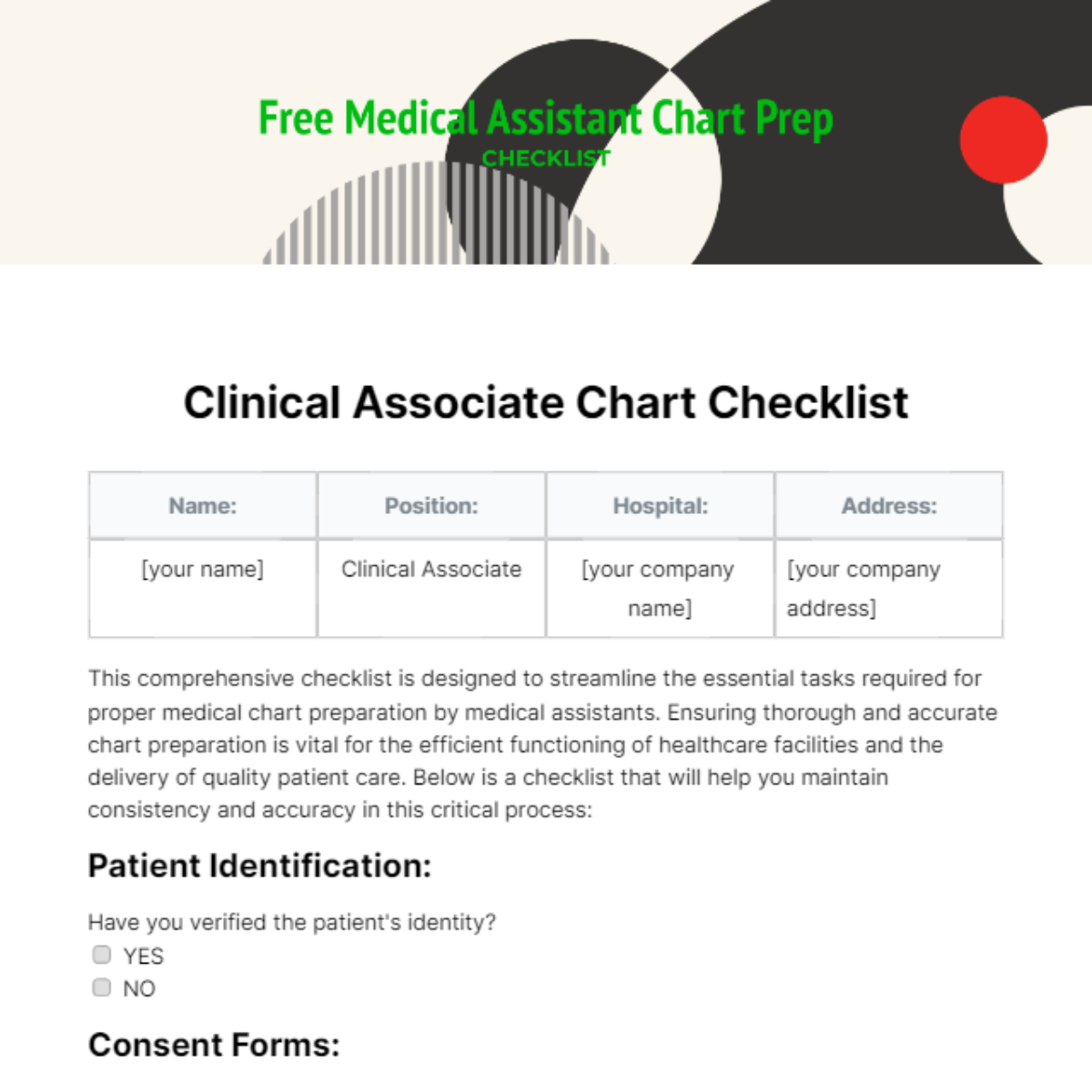
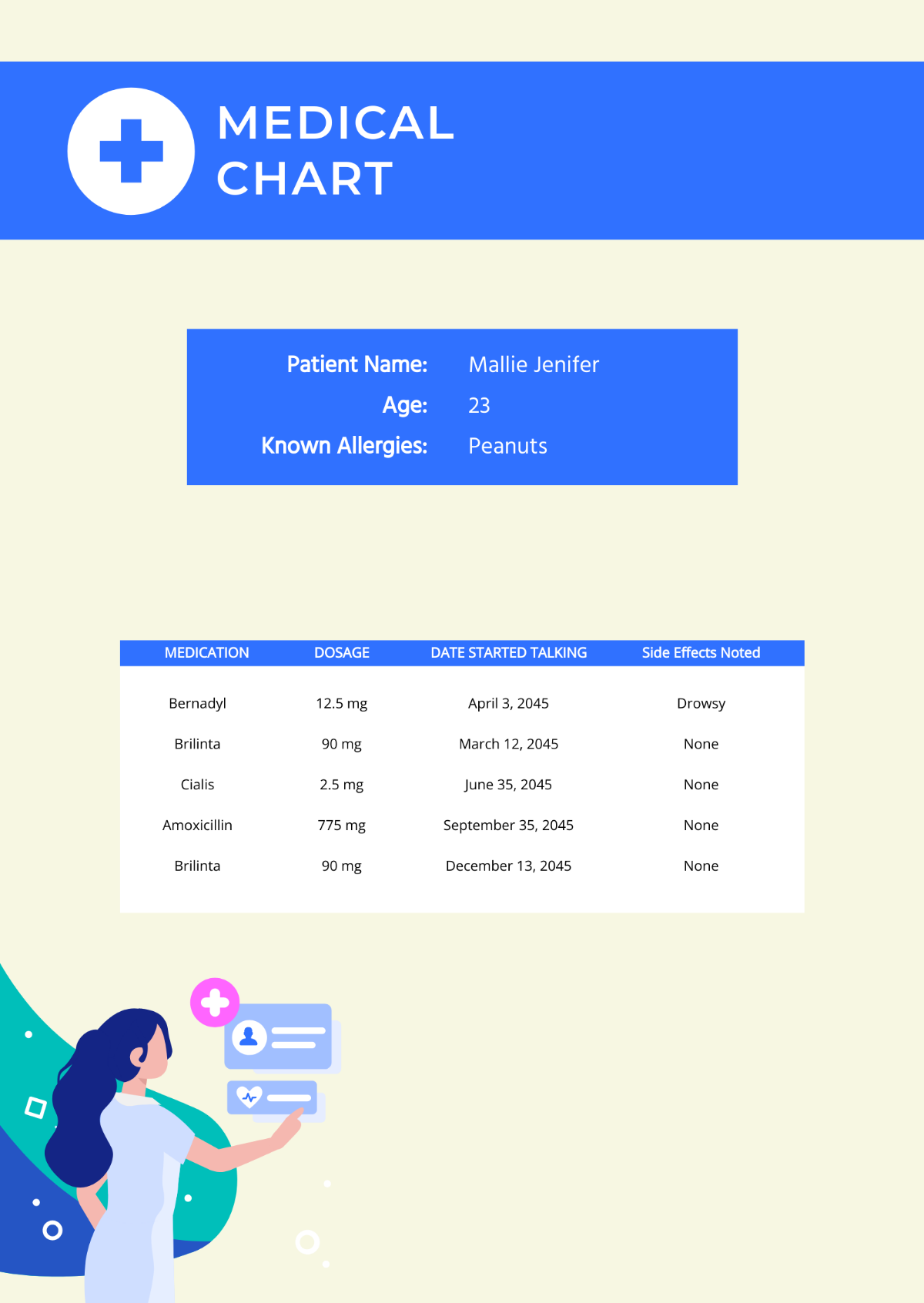
Medical Chart Layout
Prepared by: [Your Name]
Patient Information
Full Name | [Patient Full Name] |
Date of Birth | [DOB] |
Gender | [Gender] |
Contact Information | [Contact Details] |
Medical History
Narrative summary of the patient's past medical history, including any chronic conditions, past surgeries, allergies, and medications.
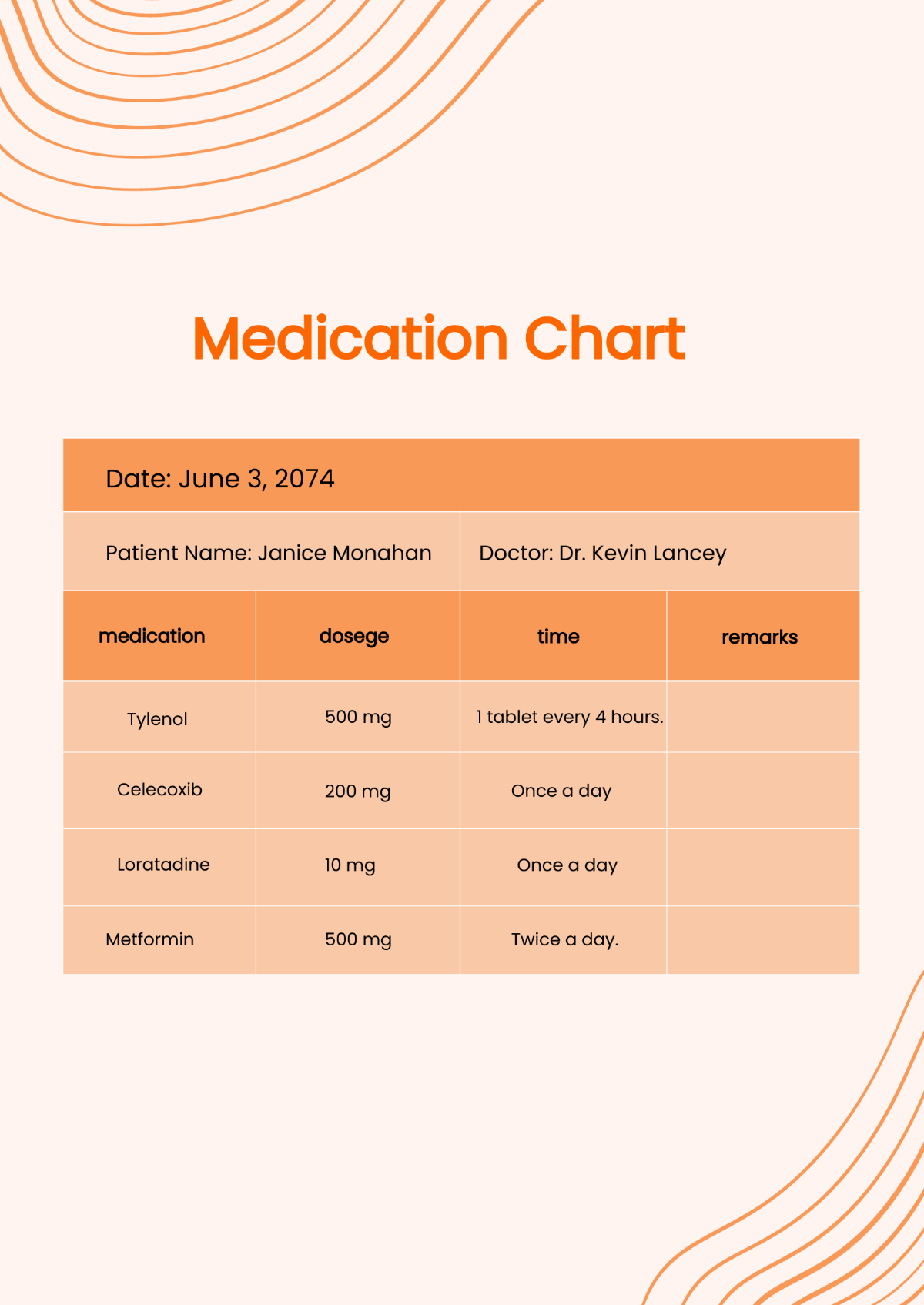
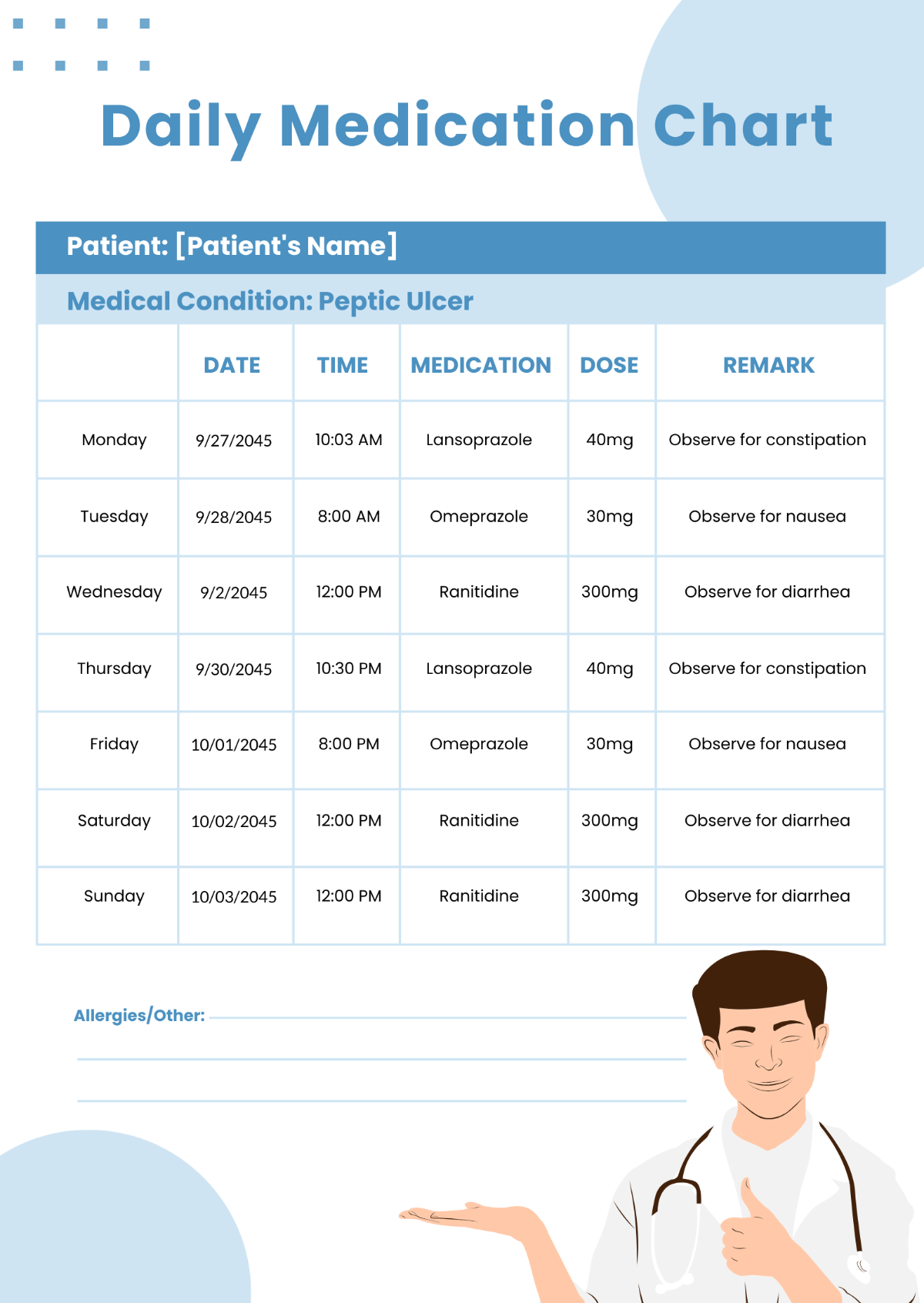
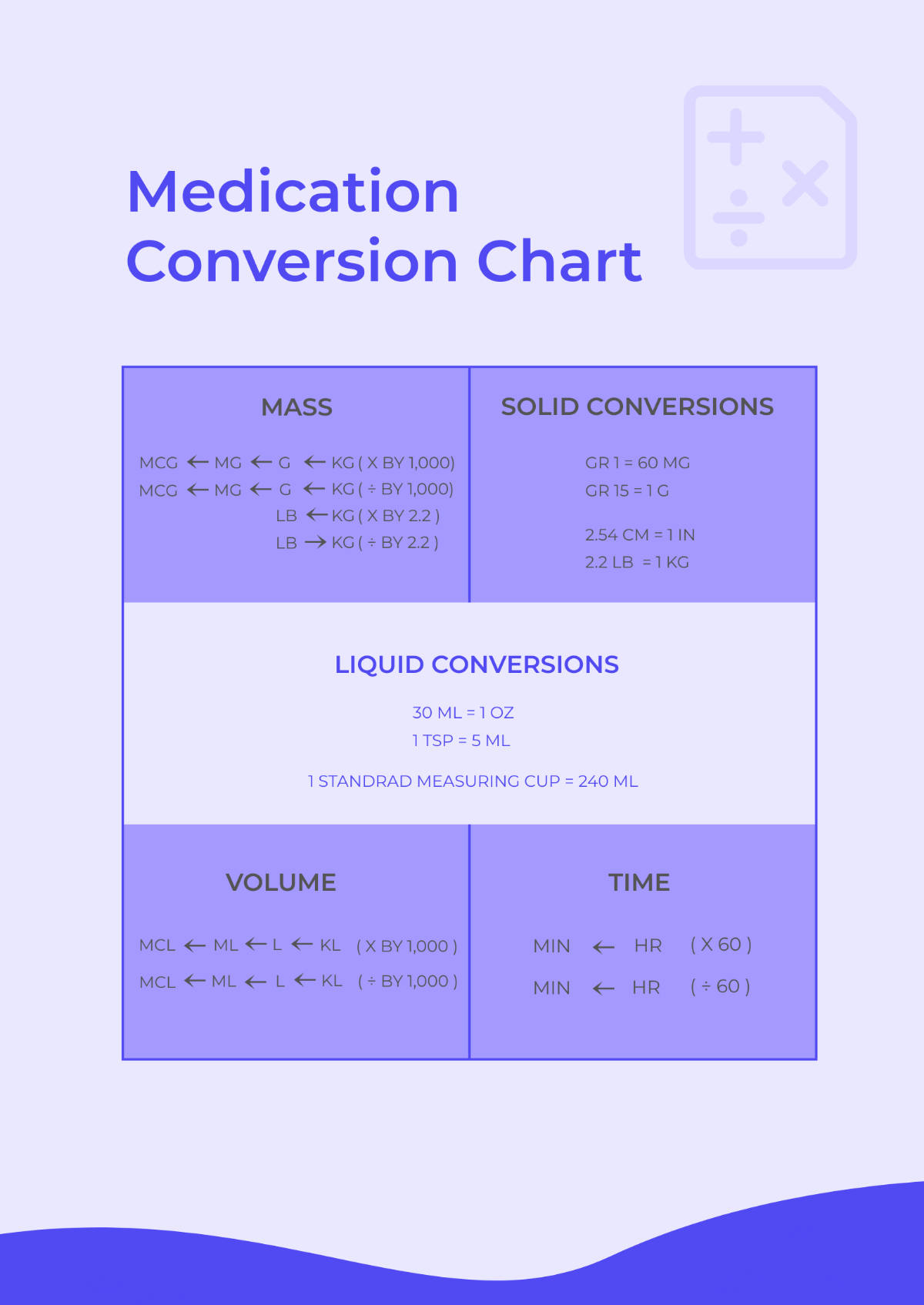
Current Medications
Medication Name | Dosage | Frequency |
|---|
[Medication 1] | [Dosage] | [Frequency] |
[Medication 2] | [Dosage] | [Frequency] |
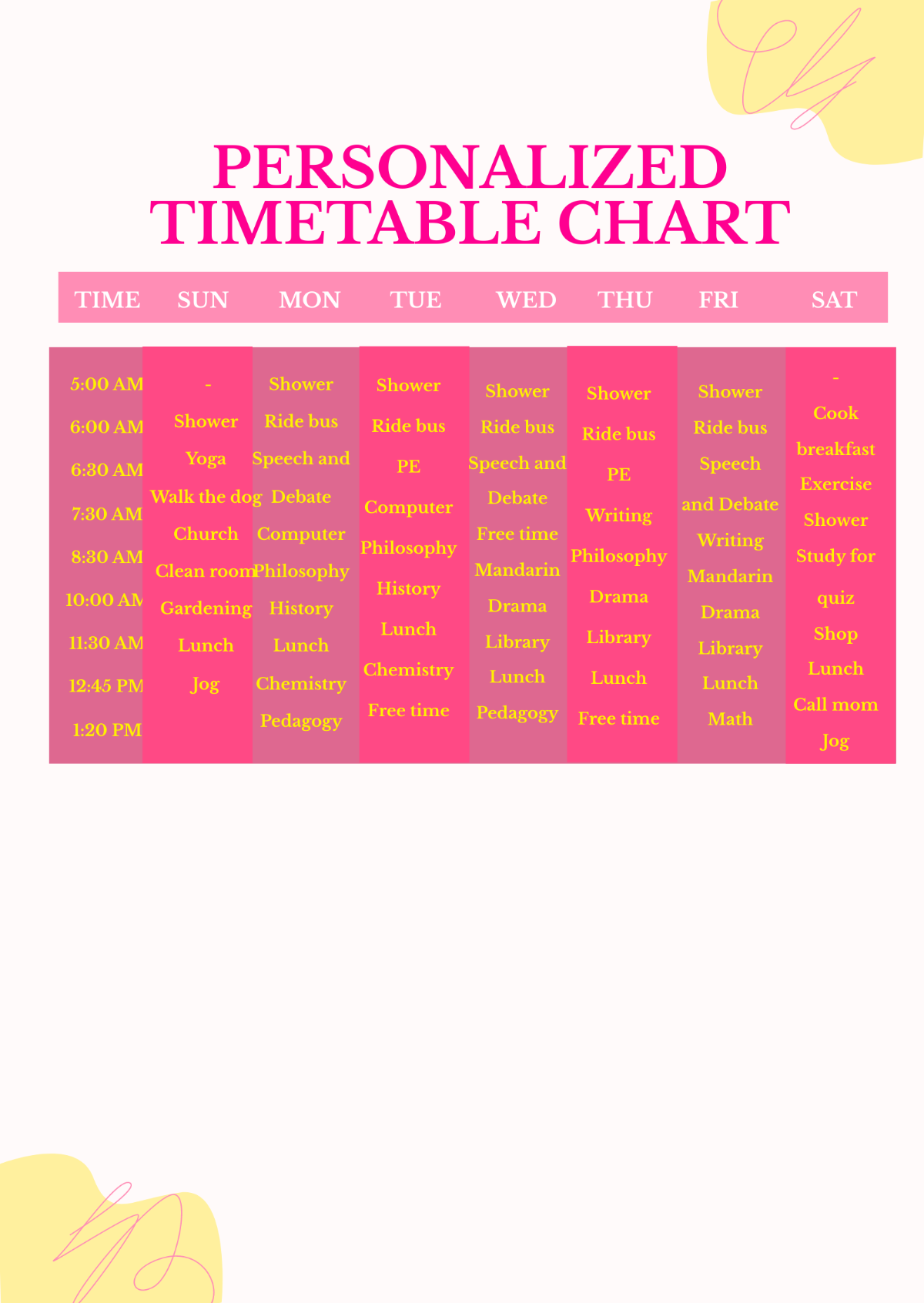
Recent Appointments
Date | Physician | Purpose | Notes |
|---|
[Date] | [Physician] | [Purpose] | [Notes] |
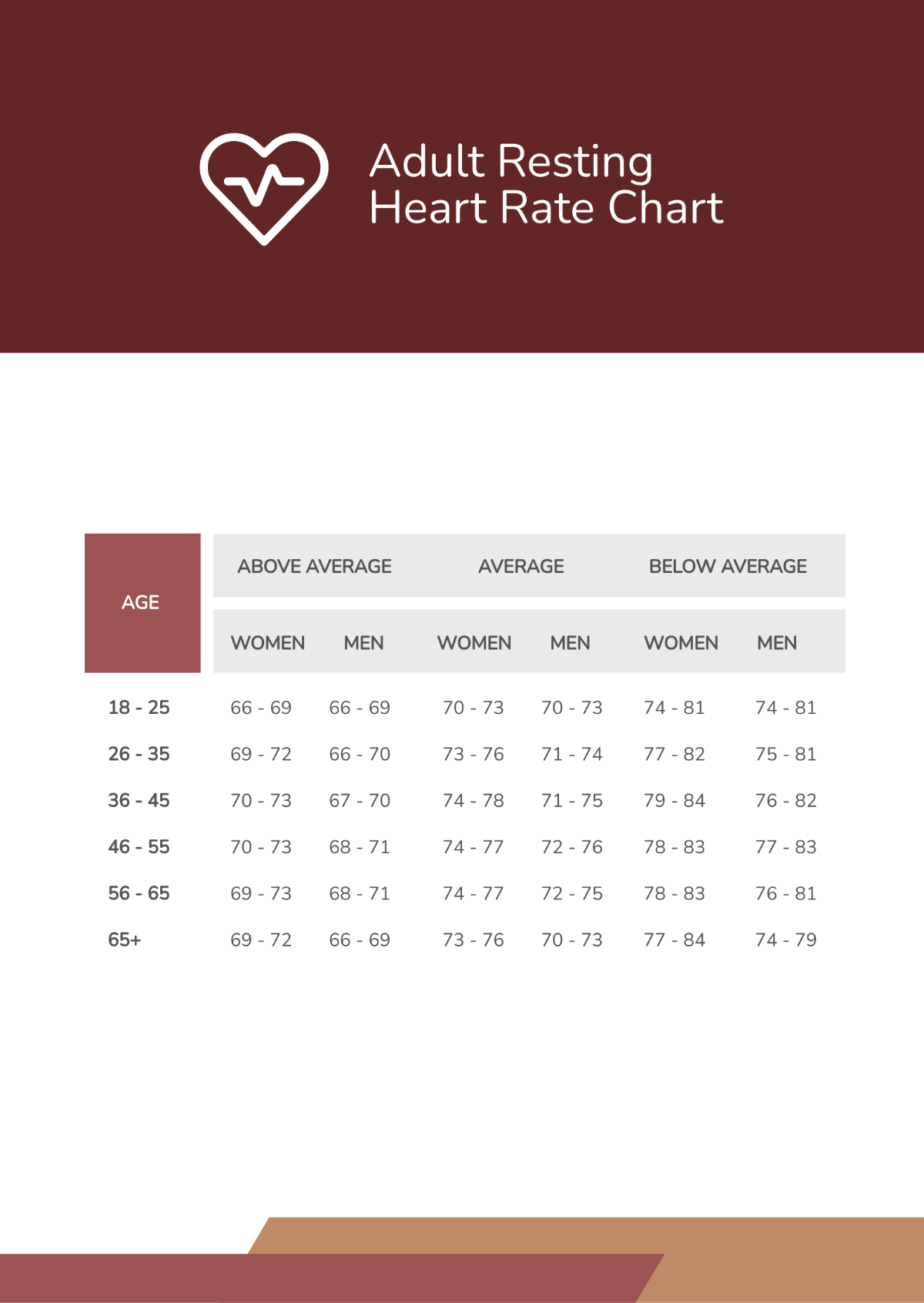
Lab Results
Summary or narrative of significant lab results, trends, and comments on the patient's current condition based on most recent tests.
Treatment Plan
Overview of the ongoing treatment plan including goals, scheduled follow-ups, and any lifestyle or dietary recommendations.
Medical Record Templates @ Template.net