Free Medical Training Needs Gap Analysis
Prepared By: [YOUR NAME]
Date: July 1, 2050
I. Current Skills and Knowledge
The initial phase in identifying training needs involves a thorough assessment of the present competency levels of medical staff. This assessment should capture a comprehensive snapshot of existing skills and knowledge, identifying strengths and areas for improvement. Typically, this evaluation includes:
Knowledge of medical procedures and protocols
Proficiency in using medical equipment and technology
Understanding of patient care methodologies
Ability to work collaboratively within multidisciplinary teams
Compliance with healthcare regulations and standards
To achieve a precise assessment, consider utilizing surveys, skills tests, direct observations, and performance reviews. The feedback from these tools will create a benchmark for evaluating current competencies versus desired outcomes.
II. Required Competencies
Defining the required competencies is crucial to establishing the criteria needed for medical staff to perform their roles effectively. Essential competencies include:
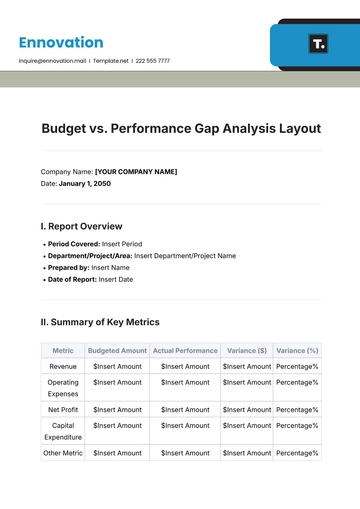
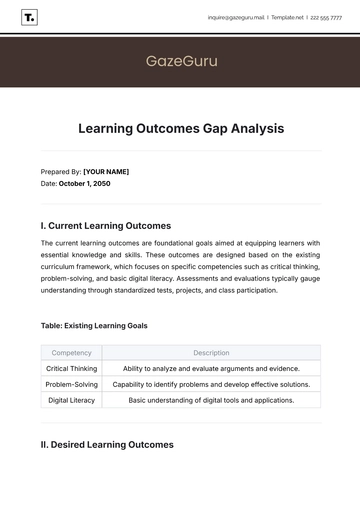
Competency | Description |
|---|---|
Clinical Expertise | Advanced knowledge of clinical procedures, disease management, and patient diagnosis. |
Technical Skills | Proficiency in operating modern medical and diagnostic equipment. |
Communication Skills | Effective interaction with patients, families, and colleagues to ensure accurate information exchange. |
Critical Thinking | Ability to analyze complex situations and make informed decisions. |
Cultural Competence | Understanding and respect for diverse patient backgrounds, ensuring sensitive care delivery. |
By outlining these competencies, we establish a foundation for training scope and objectives, ensuring alignment with organizational goals and healthcare standards.
III. Gap Analysis
The gap analysis phase involves comparing current skills and knowledge against the required competencies to identify specific areas needing improvement. This process can be conducted through SWOT analysis (Strengths, Weaknesses, Opportunities, Threats) and involves:
Identifying discrepancies between current capabilities and essential skills
Prioritizing gaps based on their impact on patient care and safety
Analyzing the root causes of these gaps, whether structural, educational, or technological
This comprehensive evaluation allows for targeted interventions, prioritizing areas that significantly affect job performance and patient outcomes.
IV. Training Recommendations
Upon identifying gaps, the next stage is recommending appropriate training programs or strategies to address these deficiencies. Recommendations may include:
Workshops and Seminars: Interactive sessions on the latest clinical practices and technologies
Online Learning Modules: Courses that are adaptable and designed to cover a wide range of fundamental topics and essential skills.
Simulation Training: Hands-on practice in a controlled environment to enhance practical skills without risk to patients.
Mentorship Programs: Guidance from experienced practitioners to foster knowledge transfer and professional development.
Continuous Professional Education (CPE): Regular sessions to stay updated with evolving medical standards and practices.
These training initiatives should be customized based on individual and departmental needs, fostering a culture of continuous improvement and learning.
V. Timeline and Resources
Implementing a training program requires a well-defined timeline and allocation of resources. Key considerations include:
Timeline: Developing a phased approach, where critical skills are addressed first. Set short-term and long-term milestones for tracking progress.
Resources: Allocation of budget, staffing, and materials necessary to support training programs. Leverage technology for e-learning and virtual simulations to optimize resource use.
Evaluation Metrics: Establishing key performance indicators (KPIs) to measure training effectiveness and integration of new competencies into practice.
A strategic plan with clear timelines and resources ensures systematic implementation, fostering enhanced clinical performance and patient care delivery.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Address skill gaps in healthcare with the Medical Training Needs Gap Analysis Template from Template.net. This editable and customizable tool evaluates current training programs and identifies areas for improvement. Modify the template effortlessly editable in our AI Editor Tool to suit your institution’s specific requirements. Enhance healthcare training and ensure competency with this essential resource.