Free Nursing Home Health Documentation
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Maintain thorough records with the Nursing Home Health Documentation Template from Template.net. This editable and customizable template supports detailed health documentation. Customize it using our Ai Editor Tool for accurate and organized health records. Stay organized—create detailed health documentation with our template!
You may also like
Nursing Home Health Documentation
Date: 2050-01-15
Nursing Facility Name: [Your Company Name]
Location: [Your Company Address]
Year: 2050
Prepared by: [Your Name]
I. Introduction
This document is intended to offer a thorough and detailed guide to nursing home health documentation practices at [Your Company Name]. It emphasizes the importance of meticulous record-keeping to ensure the highest standards of patient care, regulatory compliance, and effective communication among healthcare providers. Accurate documentation is essential for providing comprehensive and coordinated care, supporting clinical decision-making, and meeting legal and ethical standards. As healthcare continues to advance in 2050, the methods and technologies used in documentation evolve, necessitating up-to-date practices that reflect current standards.
The documentation process not only supports immediate patient care but also contributes to longitudinal health management. By maintaining detailed records, healthcare providers can track the progression of conditions, evaluate the effectiveness of interventions, and adjust care plans as needed. Furthermore, proper documentation is critical for ensuring continuity of care, especially in a nursing home setting where patients may experience frequent changes in their health status or require various types of care from multiple disciplines.
II. Patient Admission Documentation
A. Initial Assessment
The initial assessment marks the beginning of a patient’s journey at [Your Company Name] and is a pivotal moment for establishing a baseline for their health care. This comprehensive assessment is performed by a Registered Nurse (RN) or a qualified healthcare provider and is essential for creating an individualized care plan tailored to the patient's needs.
Medical History
A detailed account of the patient’s previous health conditions, including any chronic illnesses, past surgeries, and any ongoing medical treatments, must be meticulously recorded. This history should encompass information about previous hospitalizations, significant medical events, and family history of genetic or hereditary conditions that could impact the patient’s current health.
It is crucial to gather information about any allergies or adverse reactions to medications, as this information will guide safe and effective treatment planning. Any existing medical devices or implants should also be noted, as these can affect patient care and treatment options.
Physical Assessment
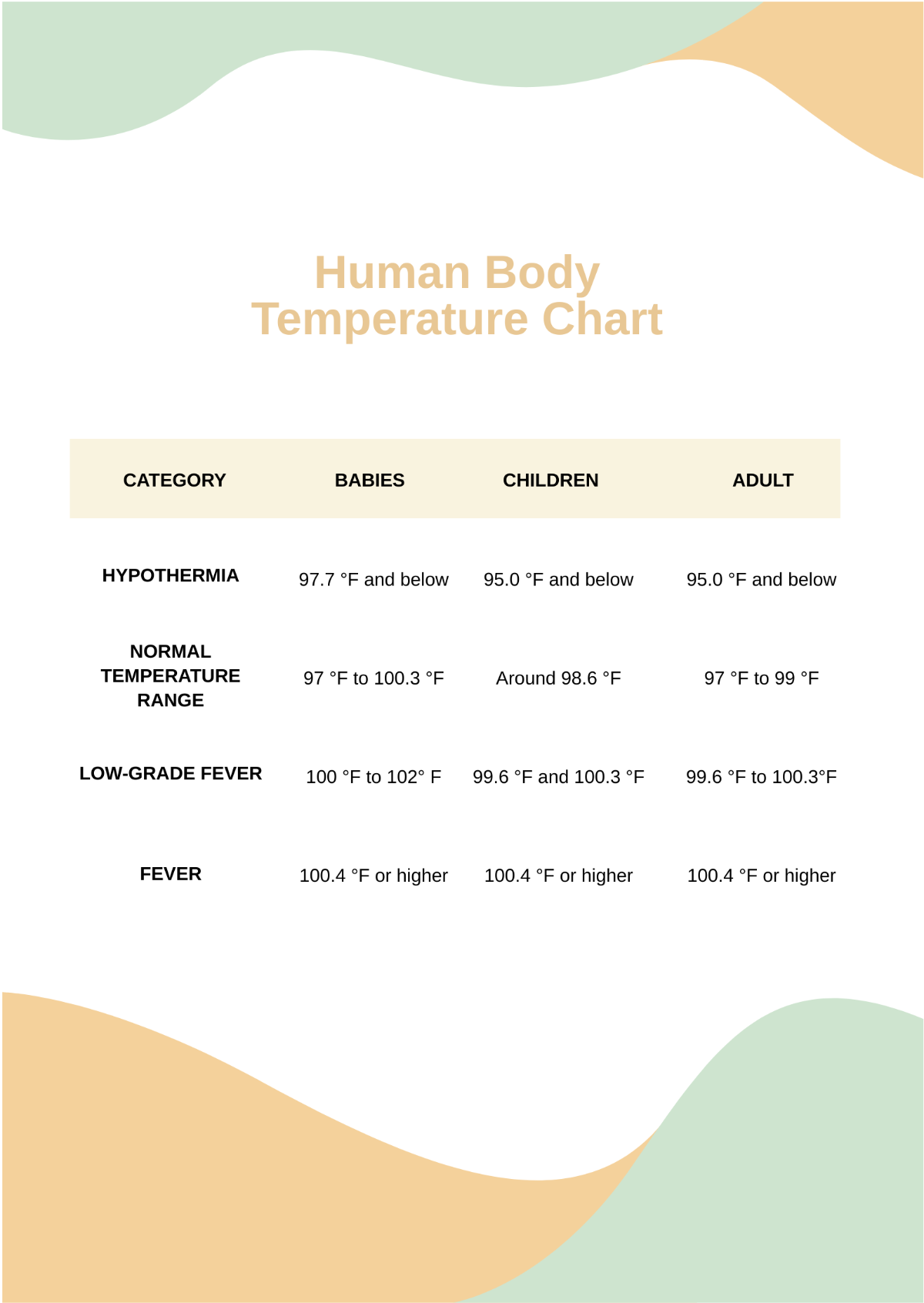
A thorough head-to-toe physical examination is conducted to assess the patient’s overall health status. This examination includes measuring vital signs—such as temperature, pulse, respiratory rate, and blood pressure—to establish baseline data and identify any immediate health concerns.
The assessment includes a detailed examination of each body system, documenting findings such as heart sounds, lung sounds, abdominal condition, and neurological status. Special attention is given to identifying any skin conditions, such as pressure ulcers or infections, which may require specialized care.
Psychosocial Assessment
Evaluating the patient’s mental and emotional well-being is critical in understanding their overall health and readiness for care. This assessment involves evaluating the patient’s cognitive function, including their memory, attention, and problem-solving abilities.
Social interactions and support systems are assessed to identify any potential needs for counseling or social support services. Documentation of any psychological conditions, such as depression or anxiety, is crucial for tailoring mental health support and interventions.
Functional Assessment
Assessing the patient’s ability to perform Activities of Daily Living (ADLs) provides insight into their functional status and independence. This includes evaluating their ability to perform tasks such as bathing, dressing, feeding themselves, and moving around their environment.
The functional assessment also involves documenting the use of any assistive devices, such as walkers or wheelchairs, and determining the need for any additional support to maintain or improve functional abilities.
Risk Assessment
Identifying potential risks is essential for developing a proactive care plan. This includes assessing fall risks, infection risks, and any other potential hazards that could impact the patient’s health and safety.
Preventative measures are documented and implemented based on the identified risks. This might include environmental modifications, such as installing grab bars, or implementing specific protocols to reduce the likelihood of infections.
B. Admission Orders
Following the initial assessment, admission orders are generated by the attending physician and are crucial for guiding the patient’s immediate and ongoing care. These orders are documented in the patient’s Electronic Health Record (EHR) and must be followed precisely to ensure optimal care delivery.
Medications
Detailed medication orders include the name of each medication, dosage, route of administration, and frequency. Any special instructions related to the medication’s administration, such as with food or specific times, are clearly documented.
Orders for controlled substances or medications with high risks of side effects require additional documentation and monitoring to ensure patient safety.
Therapeutic Interventions
Specific therapeutic interventions are ordered based on the patient’s health needs. This may include physical therapy for mobility issues, occupational therapy for activities of daily living, or speech therapy for communication challenges.
Documentation includes the type of therapy, frequency, and goals of the intervention, as well as any special equipment or techniques required.
Dietary Requirements
Dietary orders specify any special dietary needs or restrictions, such as low sodium diets for heart conditions or diabetic diets for blood sugar control. The patient’s preferences and any allergies are also documented to ensure meals are tailored to their needs.
Instructions for meal preparation, including texture modifications or specific nutrient requirements, are included to support the patient’s nutritional health.
Diagnostic Tests
Orders for diagnostic tests, such as blood work, imaging studies, or specialized evaluations, are documented to provide insight into the patient’s health status and guide treatment decisions.
The results of these tests are tracked and reviewed, with follow-up orders or adjustments to the care plan made based on the findings.
All information from the initial assessment and admission orders is recorded in the patient’s EHR, ensuring that all healthcare team members have access to current and accurate information.
III. Care Planning Documentation
A. Developing the Care Plan
The development of a personalized care plan is a collaborative process involving the patient, their family, and the multidisciplinary care team. The care plan serves as a comprehensive guide to the patient’s care, outlining specific goals and the steps needed to achieve them.
Problem Identification
The care plan begins with identifying and documenting the patient’s primary health issues. This includes chronic conditions that need ongoing management, acute issues requiring immediate attention, and any psychosocial or behavioral concerns that may impact the patient’s well-being.
Detailed documentation of each problem includes its severity, impact on daily living, and any factors that contribute to the issue, such as lifestyle or environmental factors.
Goals and Outcomes
The care plan sets clear, measurable goals for the patient’s health and well-being. These goals should be specific, achievable, and time-bound, providing a clear target for both the care team and the patient.
Short-term goals might focus on immediate improvements, such as managing pain or preventing complications, while long-term goals address broader health objectives, such as improving mobility or enhancing quality of life.
Interventions
Nursing interventions are detailed in the care plan, specifying the actions required to address the identified problems and achieve the set goals. Each intervention includes detailed instructions on how, when, and by whom it will be performed.
For example, an intervention might involve administering a specific medication at scheduled times, performing wound care using a particular technique, or providing physical therapy exercises to improve strength.
Reevaluation and Adjustment
The care plan includes provisions for regular reevaluation to assess the patient’s progress and make necessary adjustments. Reevaluation typically occurs every [30] to [90] days, depending on the patient’s needs and changes in their condition.
Adjustments to the care plan are documented, including any changes to goals, interventions, or outcomes based on the patient’s response to treatment or new developments in their health status.
B. Multidisciplinary Team Involvement
The care planning process at [Your Company Name] involves a multidisciplinary team to ensure a holistic approach to patient care. Each team member contributes their expertise to develop and implement an effective care plan.
Nursing Staff
Nursing staff are responsible for carrying out the day-to-day care outlined in the care plan, including administering medications, monitoring vital signs, and providing support for activities of daily living.
They document their observations and any changes in the patient’s condition, which are essential for adjusting the care plan and ensuring continuity of care.
Physicians
Physicians provide medical oversight and are responsible for making high-level decisions regarding treatment and care. They review the care plan and make recommendations based on the patient’s medical condition and response to treatment.
Physicians also order diagnostic tests and therapeutic interventions, ensuring that all aspects of the patient’s care are addressed.
Therapists
Physical, occupational, and speech therapists contribute to the care plan by providing specialized interventions to improve the patient’s functional abilities. They set specific therapy goals and document progress toward these goals.
Therapists collaborate with nursing staff to integrate therapeutic exercises and activities into the patient’s daily routine.
Social Workers and Psychologists
Social workers and psychologists provide support for the patient’s emotional and mental health needs. They help address issues such as coping with illness, adjusting to the nursing home environment, and managing stress.
They also assist with discharge planning, ensuring that the patient has appropriate support systems and resources in place when leaving the facility.
The multidisciplinary team’s collaboration ensures that all aspects of the patient’s health and well-being are addressed, providing comprehensive and coordinated care.
IV. Daily Documentation and Monitoring
A. Medication Administration Record (MAR)
The Medication Administration Record (MAR) is a crucial element of daily documentation, ensuring that all medications are administered accurately and on schedule. The MAR system at [Your Company Name] includes advanced features for enhanced accuracy and efficiency.
Real-Time Tracking
The MAR system tracks medication administration in real-time, providing immediate updates on medication status and any discrepancies. This ensures that medications are administered as prescribed and that any missed doses or errors are promptly addressed.
Barcode scanning technology is used to verify the medication, dose, and patient identity, reducing the risk of errors and ensuring that the right medication reaches the right patient.
Alerts and Notifications
The system includes alerts and notifications to inform nursing staff when medications are due, when there are potential drug interactions, or when a patient’s medication regimen needs adjustment.
These alerts help prevent medication errors and ensure that any issues are addressed before they impact the patient’s health.
PRN (As-Needed) Medication
Documentation of PRN medications includes the reason for administration, the patient’s response, and any subsequent actions taken. This ensures that PRN medications are used appropriately and that their effectiveness is monitored.
The system tracks the frequency and dosage of PRN medications to prevent overuse and ensure that they are administered only when necessary.
B. Shift Notes
Shift notes are essential for maintaining continuity of care between nursing shifts. These notes provide a summary of the patient’s condition and any significant events that occurred during the shift.
Changes in Condition
Any changes in the patient’s health status, such as new symptoms, alterations in vital signs, or unexpected changes in behavior, are documented in shift notes. This information is critical for ongoing care planning and intervention.
Detailed notes help identify trends or patterns in the patient’s condition, enabling the care team to make informed decisions and adjust the care plan as needed.
Interventions Performed
Shift notes include documentation of all interventions performed during the shift, such as wound care, medication administration, or dietary changes. This ensures that all aspects of the patient’s care are recorded and that any issues are addressed promptly.
Notes also include information about the patient’s response to interventions, which is important for evaluating their effectiveness and making any necessary adjustments.
Patient-Staff Interaction
Documentation of interactions between the patient and staff provides insight into the patient’s emotional and psychological state. This includes notes on any refusals of care, behavioral issues, or positive interactions that may impact the patient’s overall well-being.
Understanding these interactions helps the care team tailor their approach to the patient’s needs and preferences.
C. Vital Signs Monitoring
Monitoring vital signs is a key component of daily documentation, providing essential data on the patient’s health status. At [Your Company Name], advanced technology is used to ensure accurate and continuous monitoring.
Blood Pressure
Blood pressure is measured regularly to detect any deviations from normal ranges and to monitor the effectiveness of treatments for conditions such as hypertension.
Regular monitoring helps identify potential issues early and allows for timely interventions to manage blood pressure effectively.
Heart Rate and Pulse
Continuous monitoring of heart rate and pulse provides real-time data on the patient’s cardiovascular health. Wearable technology tracks these parameters and alerts staff to any irregularities or significant changes.
This data is used to assess the patient’s response to treatments and to identify any potential issues that may require further evaluation.
Temperature
Temperature is monitored routinely to detect any signs of infection or other health issues. Increased frequency of temperature checks may be required if the patient shows symptoms of illness or has a known infection.
Accurate temperature monitoring helps ensure that any fever or abnormal temperature readings are addressed promptly.
Respiratory Rate
Respiratory rate and oxygen saturation levels are monitored, especially in patients with respiratory conditions or those at risk of respiratory complications. Continuous monitoring helps detect any changes in breathing patterns and allows for timely interventions.
Documentation includes any adjustments to oxygen therapy or respiratory treatments based on the patient’s needs.
V. Incident Reporting and Documentation
A. Falls and Accidents
Falls and accidents are significant events that require thorough documentation to ensure patient safety and to prevent future incidents. Accurate incident reporting is crucial for identifying trends and implementing preventive measures.
Description of the Incident
A detailed description of the incident includes the time, location, and circumstances leading up to the event. This information helps identify potential contributing factors and areas for improvement.
Documentation should also include any immediate actions taken to address the incident, such as first aid or emergency response.
Injuries Sustained
Any injuries sustained during the incident are documented, including their severity, location, and any treatment provided. This information is important for assessing the impact of the incident on the patient’s health and for planning any necessary follow-up care.
Detailed injury documentation helps track the recovery process and evaluate the effectiveness of any interventions.
Preventive Measures
Following an incident, an analysis is conducted to identify why the event occurred and what can be done to prevent similar incidents in the future. This may involve modifying the environment, changing procedures, or implementing new safety protocols.
Documentation of preventive measures includes any changes made to reduce the risk of future incidents, such as enhanced staff training or environmental modifications.
B. Adverse Medication Reactions
Adverse reactions to medication require prompt documentation to ensure patient safety and to guide future treatment decisions. Thorough documentation helps identify patterns and prevent recurrence of similar reactions.
Symptoms
A detailed account of the symptoms experienced by the patient is recorded, including their onset, duration, and severity. This information is crucial for diagnosing the reaction and determining appropriate treatment.
Documentation should also include any specific triggers or factors that may have contributed to the adverse reaction.
Response
The response to the adverse reaction is documented, including any immediate actions taken to address the issue, such as administering antidotes or discontinuing the medication.
Follow-up care is also documented, including monitoring the patient’s recovery and any additional treatments or interventions required.
Follow-Up
Ongoing monitoring and documentation of the patient’s condition are essential to ensure recovery from the adverse reaction and to prevent future occurrences. This includes tracking any long-term effects and adjusting the patient’s care plan as needed.
Documentation of follow-up actions helps ensure that all aspects of the patient’s recovery are addressed and that appropriate measures are in place to prevent similar reactions.
VI. Regulatory Compliance and Audits
A. Legal and Ethical Documentation
At [Your Company Name], adherence to legal and ethical standards is paramount for maintaining the integrity of patient care and ensuring compliance with regulations. Proper documentation practices support these standards and contribute to high-quality care.
HIPAA Compliance
All patient records are kept confidential and secure, in accordance with the Health Insurance Portability and Accountability Act (HIPAA). This includes ensuring that only authorized personnel have access to sensitive information and that all data is protected from unauthorized access or breaches.
Regular audits are conducted to ensure compliance with HIPAA regulations and to address any potential vulnerabilities in the system.
State and Federal Regulations
Documentation practices are aligned with both state-specific nursing home regulations and federal laws governing long-term care facilities. This includes adhering to requirements for record-keeping, reporting, and patient rights.
Compliance with these regulations is monitored through regular reviews and updates to documentation practices as needed.
Ethical Standards
Documentation must be accurate, truthful, and completed in a timely manner. Any falsification or omission of information is strictly prohibited and can have serious consequences for patient care and regulatory compliance.
Ethical standards are reinforced through training and ongoing education for all staff members, ensuring that they understand and adhere to best practices in documentation.
B. Audits and Reviews
Regular internal and external audits are conducted to ensure that documentation practices meet the required standards and to identify areas for improvement. These audits play a crucial role in maintaining high-quality care and compliance.
Patient Records
Auditors review patient records for completeness and accuracy, checking that all required documentation is present and properly maintained. This includes verifying that assessments, care plans, and progress notes are up-to-date and reflect the patient’s current condition.
Any discrepancies or missing information are addressed, and corrective actions are implemented to ensure that documentation practices are improved.
Care Plans
Audits focus on whether care plans are regularly updated and accurately reflect the patient’s needs and progress. This includes evaluating the alignment of goals, interventions, and outcomes with the patient’s health status.
Feedback from audits is used to refine care planning processes and ensure that care plans are comprehensive and effective.
Incident Reports
Auditors examine incident reports to ensure that they are thorough and accurately documented. This includes reviewing the description of the incident, the actions taken, and the preventive measures implemented.
Trends or patterns identified during audits are addressed through policy changes or staff training to prevent future incidents.
VII. Discharge and Transfer Documentation
A. Discharge Summary
A comprehensive discharge summary is prepared when a patient is discharged from [Your Company Name], providing a detailed overview of their health status and care needs. This summary is crucial for ensuring a smooth transition from the nursing home to the next stage of care.
Reason for Discharge
The reason for discharge is documented, including whether the patient is leaving due to recovery, transfer to another facility, or other reasons such as personal choice or end-of-life care.
Any relevant details about the discharge decision are included to provide context and support continuity of care.
Patient Condition
The discharge summary includes a summary of the patient’s condition at the time of discharge, including any ongoing health concerns or issues that need to be addressed.
This information helps ensure that the next care provider is fully informed about the patient’s health status and needs.
Follow-Up Care
Documentation of follow-up care includes any appointments with specialists, home healthcare services, or physical therapy that are required after discharge.
Instructions for follow-up care are clear and detailed, providing the patient and their family with all necessary information to manage their care effectively.
B. Transfer Documentation
When a patient is transferred to another healthcare facility, all relevant documentation is promptly and accurately transferred to ensure continuity of care.
Transfer Orders
Transfer orders include detailed instructions for the patient’s care, including medications, treatments, and any immediate needs. This information ensures that the receiving facility can provide appropriate care from the moment of transfer.
Documentation of any special considerations or precautions is included to ensure that the patient’s needs are fully addressed.
Patient History
A comprehensive summary of the patient’s medical history is provided, including recent treatments, lab results, and progress notes. This information helps the receiving facility understand the patient’s background and current health status.
Any ongoing issues or concerns are highlighted to ensure that the receiving facility is aware of and prepared to address them.