Free Clinical Incident Report
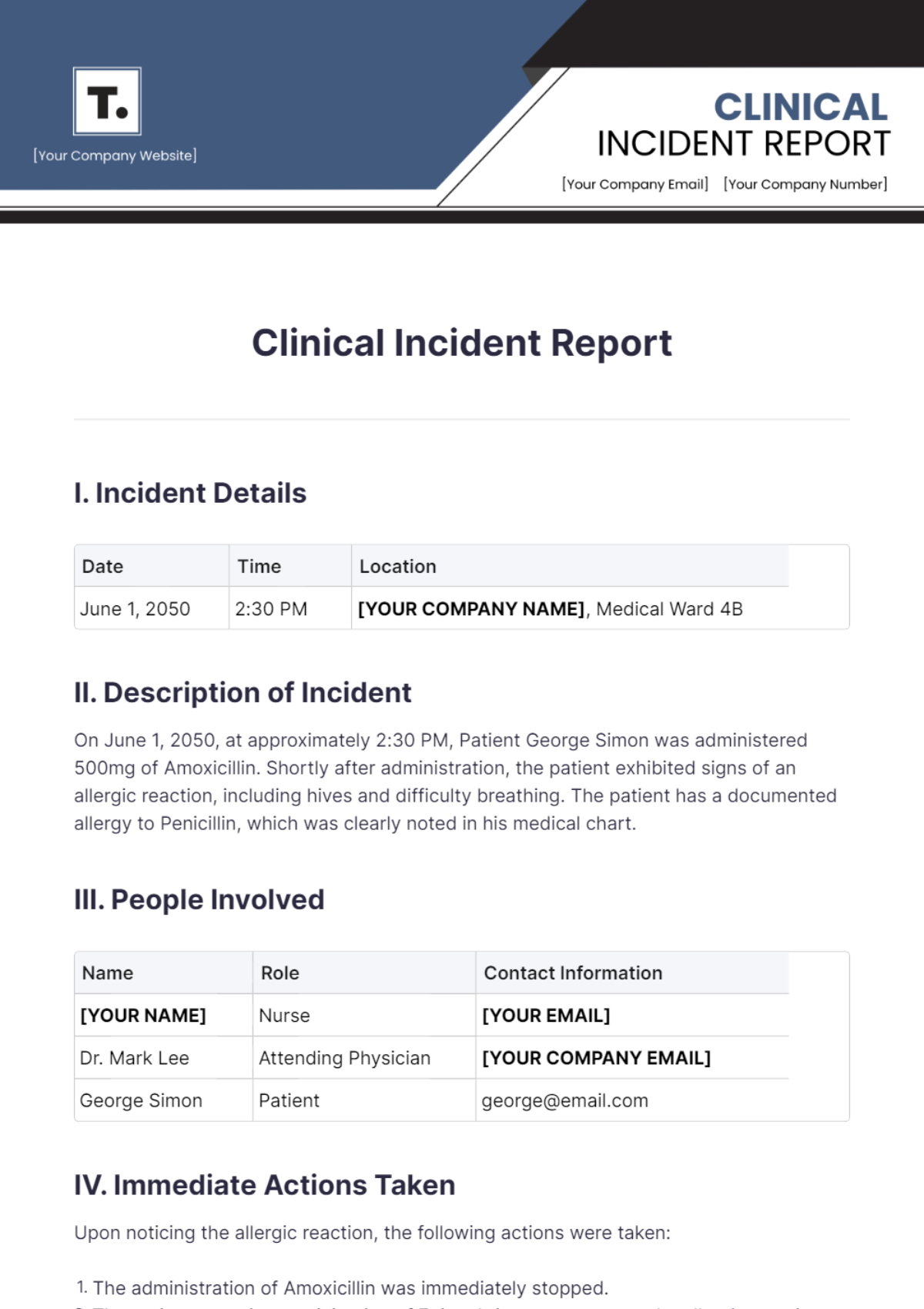
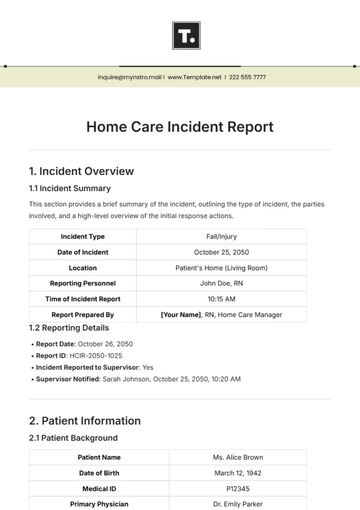
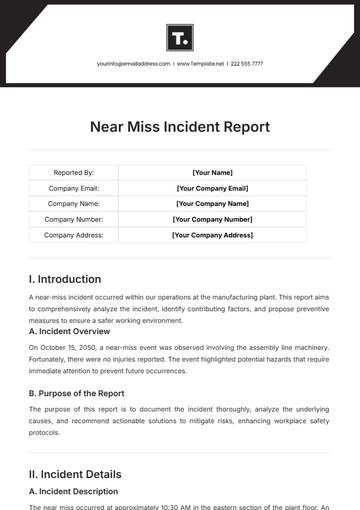
I. Incident Details
Date | Time | Location |
|---|---|---|
June 1, 2050 | 2:30 PM | [YOUR COMPANY NAME], Medical Ward 4B |
II. Description of Incident
On June 1, 2050, at approximately 2:30 PM, Patient George Simon was administered 500mg of Amoxicillin. Shortly after administration, the patient exhibited signs of an allergic reaction, including hives and difficulty breathing. The patient has a documented allergy to Penicillin, which was clearly noted in his medical chart.
III. People Involved
Name | Role | Contact Information |
|---|---|---|
[YOUR NAME] | Nurse | [YOUR EMAIL] |
Dr. Mark Lee | Attending Physician | [YOUR COMPANY EMAIL] |
George Simon | Patient | george@email.com |
IV. Immediate Actions Taken
Upon noticing the allergic reaction, the following actions were taken:
The administration of Amoxicillin was immediately stopped.
The patient was given an injection of Epinephrine to counteract the allergic reaction.
Dr. Mark Lee was notified and provided immediate medical attention.
The patient was monitored closely for any further adverse reactions.
The incident was reported to the hospital's quality and risk management team.
V. Root Cause Analysis
A thorough review of the incident revealed the following contributing factors:
The medication order was entered incorrectly into the electronic health record (EHR) system.
The nurse administering the medication did not cross-check the patient's allergy information in the EHR before administration.
VI. Recommendations
To prevent similar incidents in the future, the following recommendations are made:
EHR System Alerts: Implement an automatic alert system in the EHR that flags any medication orders containing allergens listed in the patient's chart.
Double-Check Protocols: Enforce a mandatory double-check procedure for all medication administrations, especially for patients with known allergies.
Staff Training: Conduct regular training sessions for all healthcare staff on the importance of verifying allergy information before administering any medication.
Audit Procedures: Perform regular audits of medication administration records to ensure compliance with safety protocols.
VII. Signatures

[YOUR NAME], Nurse
June 1, 2050

Dr. Mark Lee, Attending Physician
June 1, 2050

Mr. Eric Berry, Quality Officer/Reviewer
June 1, 2050
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Ensure thorough and accurate documentation of clinical incidents with Template.net's Clinical Incident Report Template. Highly customizable and editable in our Ai Editor Tool, it provides a structured and detailed format that facilitates effective incident reporting, thereby enhancing patient safety and ensuring compliance with healthcare regulations. Make this template yours now!
You may also like
- Sales Report
- Daily Report
- Project Report
- Business Report
- Weekly Report
- Incident Report
- Annual Report
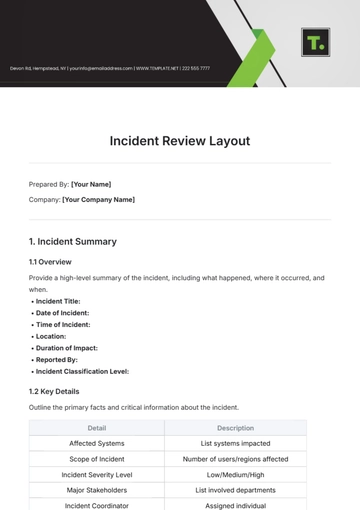
- Report Layout
- Report Design
- Progress Report
- Marketing Report
- Company Report
- Monthly Report
- Audit Report
- Status Report
- School Report
- Reports Hr
- Management Report
- Project Status Report
- Handover Report
- Health And Safety Report
- Restaurant Report
- Construction Report
- Research Report
- Evaluation Report
- Investigation Report
- Employee Report
- Advertising Report
- Weekly Status Report
- Project Management Report
- Finance Report
- Service Report
- Technical Report
- Meeting Report
- Quarterly Report
- Inspection Report
- Medical Report
- Test Report
- Summary Report
- Inventory Report
- Valuation Report
- Operations Report
- Payroll Report
- Training Report
- Job Report
- Case Report
- Performance Report
- Board Report
- Internal Audit Report
- Student Report
- Monthly Management Report
- Small Business Report
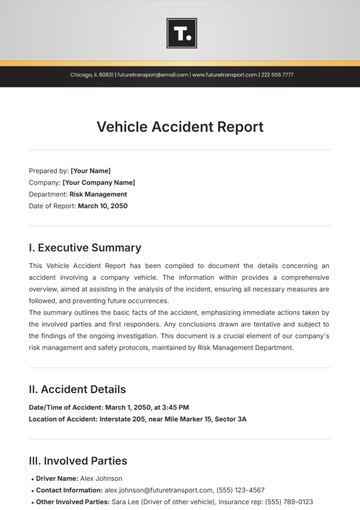
- Accident Report
- Call Center Report
- Activity Report
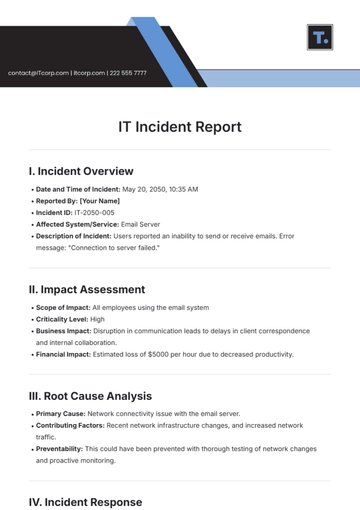
- IT and Software Report
- Internship Report
- Visit Report
- Product Report
- Book Report
- Property Report
- Recruitment Report
- University Report
- Event Report
- SEO Report
- Conference Report
- Narrative Report
- Nursing Home Report
- Preschool Report
- Call Report
- Customer Report
- Employee Incident Report
- Accomplishment Report
- Social Media Report
- Work From Home Report
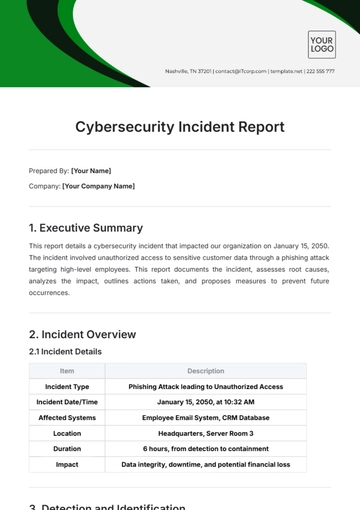
- Security Report
- Damage Report
- Quality Report
- Internal Report
- Nurse Report
- Real Estate Report
- Hotel Report
- Equipment Report
- Credit Report
- Field Report
- Non Profit Report
- Maintenance Report
- News Report
- Survey Report
- Executive Report
- Law Firm Report
- Advertising Agency Report
- Interior Design Report
- Travel Agency Report
- Stock Report
- Salon Report
- Bug Report
- Workplace Report
- Action Report
- Investor Report
- Cleaning Services Report
- Consulting Report
- Freelancer Report
- Site Visit Report
- Trip Report
- Classroom Observation Report
- Vehicle Report
- Final Report
- Software Report