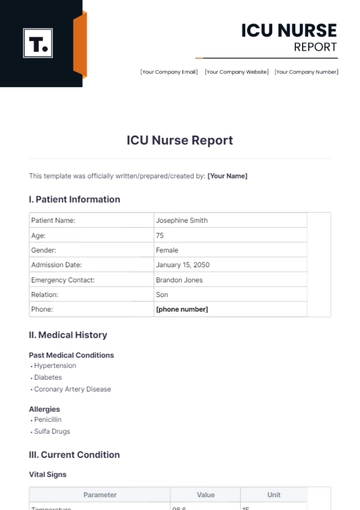
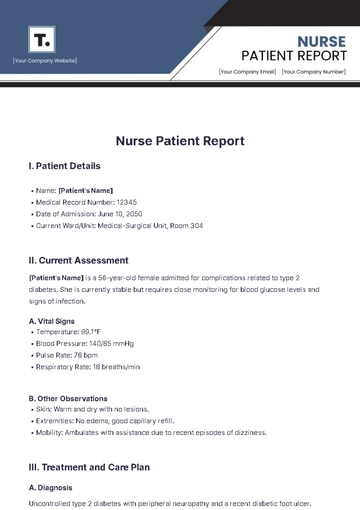
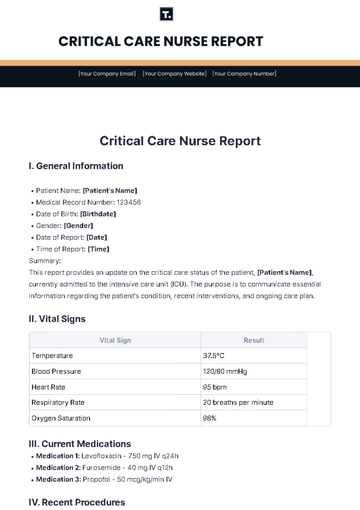
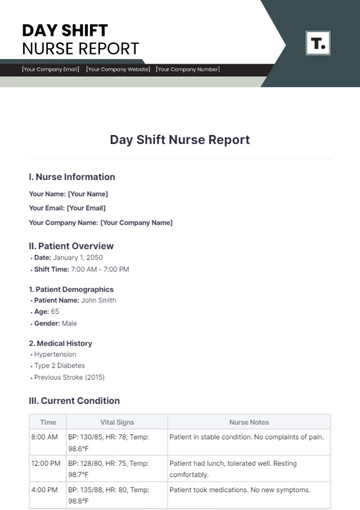
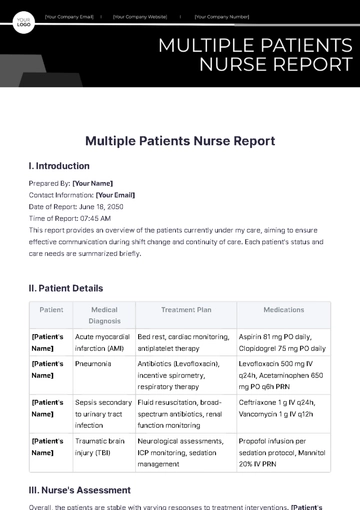
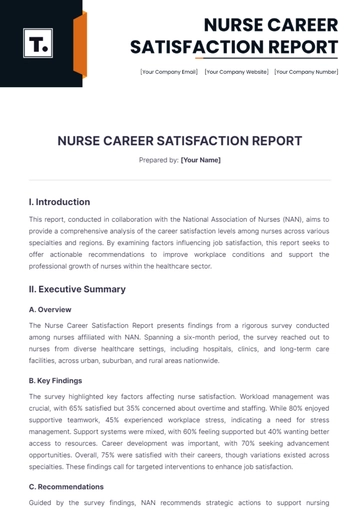
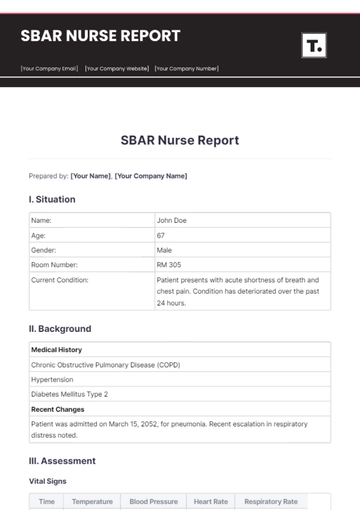
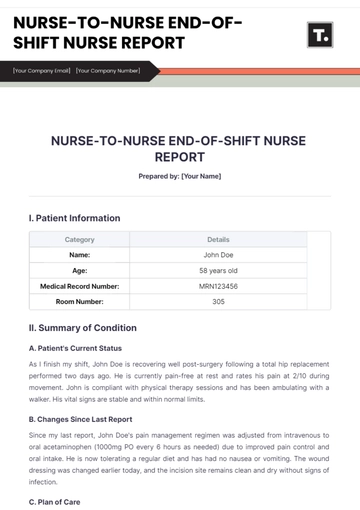
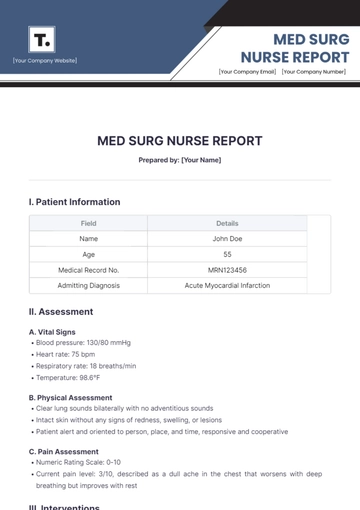
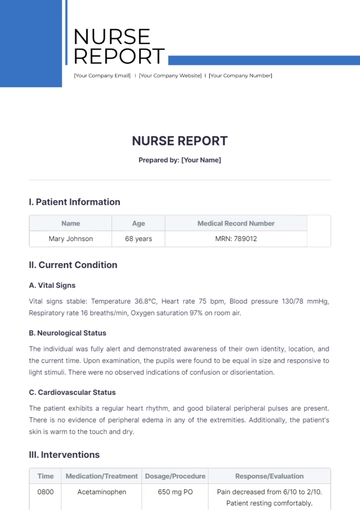
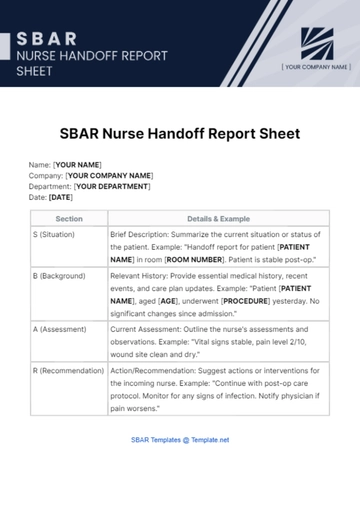
Free Nurse Report
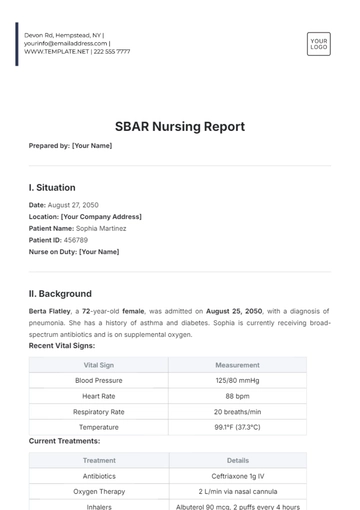
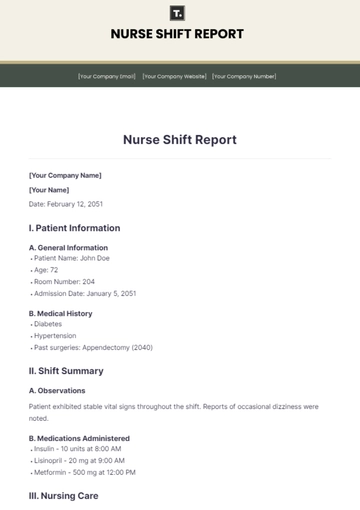
Prepared by: [Your Name]
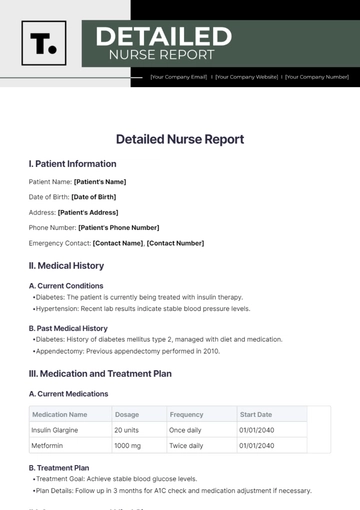
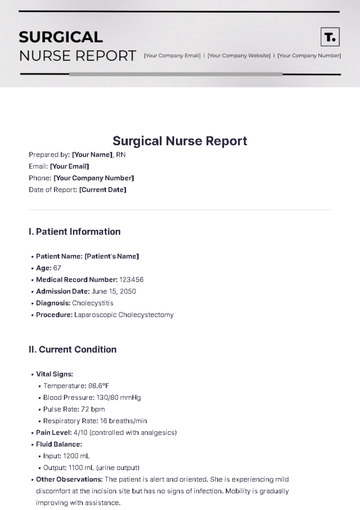
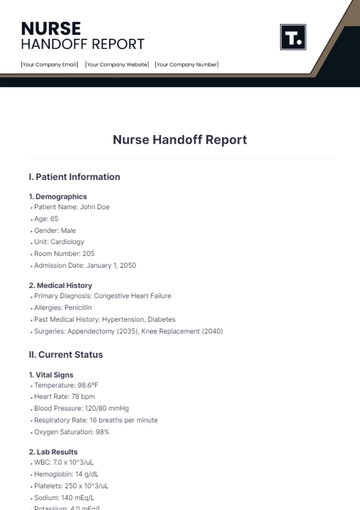
I. Patient Information
Name | Age | Medical Record Number |
|---|---|---|
Mary Johnson | 68 years | MRN: 789012 |
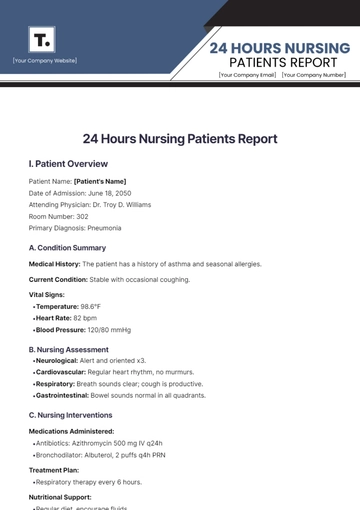
II. Current Condition
A. Vital Signs
Vital signs stable: Temperature 36.8°C, Heart rate 75 bpm, Blood pressure 130/78 mmHg, Respiratory rate 16 breaths/min, Oxygen saturation 97% on room air.
B. Neurological Status
The individual was fully alert and demonstrated awareness of their own identity, location, and the current time. Upon examination, the pupils were found to be equal in size and responsive to light stimuli. There were no observed indications of confusion or disorientation.
C. Cardiovascular Status
The patient exhibits a regular heart rhythm, and good bilateral peripheral pulses are present. There is no evidence of peripheral edema in any of the extremities. Additionally, the patient's skin is warm to the touch and dry.
III. Interventions
Time | Medication/Treatment | Dosage/Procedure | Response/Evaluation |
|---|---|---|---|
0800 | Acetaminophen | 650 mg PO | Pain decreased from 6/10 to 2/10. Patient resting comfortably. |
0900 | Insulin | Reg insulin 10U SC | Blood glucose decreased from 250 mg/dL to 150 mg/dL post-administration. |
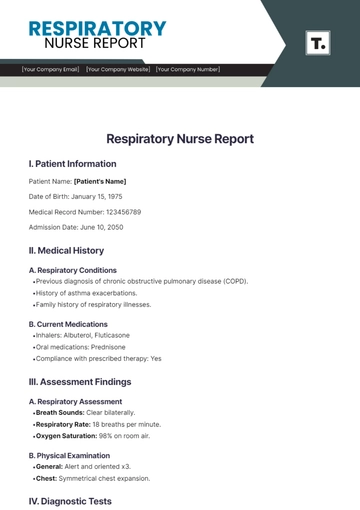
IV. Assessments
A. Respiratory Assessment
Upon examination, the patient's lungs were found to be clear upon auscultation on both the left and right sides. The oxygen saturation level was stable at 97% while breathing room air. Additionally, there were no observed signs of coughing or respiratory distress.
B. Skin Assessment
The patient’s skin was thoroughly examined and found to be intact, displaying no signs of redness, swelling, or breakdown. Upon inspection, the skin turgor was determined to be in good condition, indicating adequate hydration and elasticity. After carefully turning the patient and reassessing their skin condition, no signs of pressure injuries or other abnormalities were observed.
C. Pain Assessment
The patient has reported experiencing mild discomfort localized in the lower back region. The intensity of the pain has been quantified as a 2 out of 10 on the pain scale, indicating a relatively low level of discomfort. The administration of acetaminophen has proven effective in alleviating the patient's pain. A follow-up reassessment to evaluate the patient's pain level has been scheduled to take place in four hours.
V. Concerns
A. Clinical Concerns
The patient reported experiencing mild dizziness when they stood up this morning. After the patient rested and received adequate hydration, their vital signs remained within normal limits and appeared stable. It is recommended that the patient be monitored for orthostatic hypotension to ensure that there are no further complications or recurring symptoms related to a drop in blood pressure upon standing.
B. Family Concerns
The family members of the patient are expressing concern regarding the necessary modifications to the patient's diet and the administration of insulin. To address these concerns, comprehensive education was provided, which included detailed instructions on how to properly monitor the patient's blood glucose levels. Additionally, they were educated on the various signs and symptoms of hypoglycemia, so they can recognize and respond to them promptly.
C. Nursing Concerns
I have requested additional wound care supplies and we are currently awaiting restocking from the supply department. Additionally, there is a need for an updated nutritional assessment to better address the patient's dietary requirements.
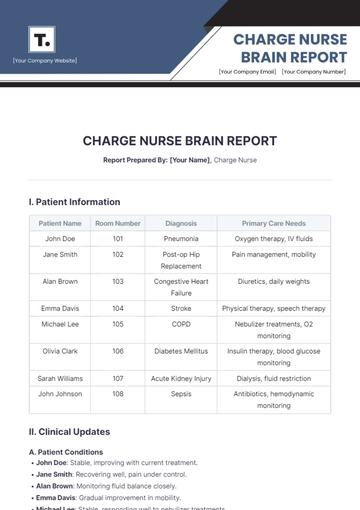
VI. Plan of Care
Intervention | Timeline |
|---|---|
Monitor blood glucose levels | Before meals and bedtime |
Assist with ambulation and fall prevention | Every 2 hours |
Provide skin care and reassessment | Every shift change |
VII. Instructions
Recipient | Instructions |
|---|---|
Patient | Continue with prescribed medications and monitor blood sugar levels closely. Follow dietary recommendations provided. |
Family | Review diet plan and encourage balanced meals. Monitor for signs of low blood sugar and report any concerns to nursing staff. |
Nursing Assistant | Assist with toileting every 2 hours and ensure patient safety during transfers. Use pressure-relieving techniques during repositioning. |
VIII. Recommendation
To address the concerns of the patient and their family about dietary modifications, it is advisable to seek consultation with a dietitian. During this consultation, the dietitian can provide professional advice and tailored plans to meet the specific dietary needs of the patient. Additionally, it is important to carefully evaluate the patient's response to their current insulin regimen. This involves closely monitoring their blood glucose levels and assessing their overall health and well-being. If any adjustments are needed based on this evaluation, modifications should be made to the insulin regimen in order to ensure that the patient maintains optimal blood glucose control.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
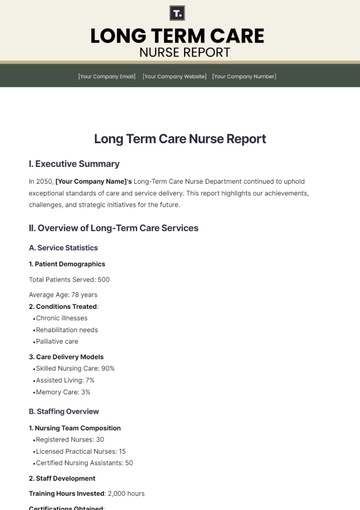
Streamline your nursing reports with the Nurse Report Template from Template.net. This fully customizable and editable template simplifies documentation, ensuring accuracy and efficiency. Editable in our AI Editor Tool, it allows seamless adjustments to meet specific needs. Enhance your workflow and save time with this user-friendly and professional template.
You may also like
- Sales Report
- Daily Report
- Project Report
- Business Report
- Weekly Report
- Incident Report
- Annual Report
- Report Layout
- Report Design
- Progress Report
- Marketing Report
- Company Report
- Monthly Report
- Audit Report
- Status Report
- School Report
- Reports Hr
- Management Report
- Project Status Report
- Handover Report
- Health And Safety Report
- Restaurant Report
- Construction Report
- Research Report
- Evaluation Report
- Investigation Report
- Employee Report
- Advertising Report
- Weekly Status Report
- Project Management Report
- Finance Report
- Service Report
- Technical Report
- Meeting Report
- Quarterly Report
- Inspection Report
- Medical Report
- Test Report
- Summary Report
- Inventory Report
- Valuation Report
- Operations Report
- Payroll Report
- Training Report
- Job Report
- Case Report
- Performance Report
- Board Report
- Internal Audit Report
- Student Report
- Monthly Management Report
- Small Business Report
- Accident Report
- Call Center Report
- Activity Report
- IT and Software Report
- Internship Report
- Visit Report
- Product Report
- Book Report
- Property Report
- Recruitment Report
- University Report
- Event Report
- SEO Report
- Conference Report
- Narrative Report
- Nursing Home Report
- Preschool Report
- Call Report
- Customer Report
- Employee Incident Report
- Accomplishment Report
- Social Media Report
- Work From Home Report
- Security Report
- Damage Report
- Quality Report
- Internal Report
- Nurse Report
- Real Estate Report
- Hotel Report
- Equipment Report
- Credit Report
- Field Report
- Non Profit Report
- Maintenance Report
- News Report
- Survey Report
- Executive Report
- Law Firm Report
- Advertising Agency Report
- Interior Design Report
- Travel Agency Report
- Stock Report
- Salon Report
- Bug Report
- Workplace Report
- Action Report
- Investor Report
- Cleaning Services Report
- Consulting Report
- Freelancer Report
- Site Visit Report
- Trip Report
- Classroom Observation Report
- Vehicle Report
- Final Report
- Software Report