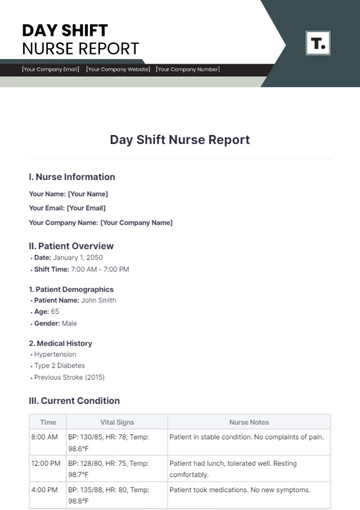
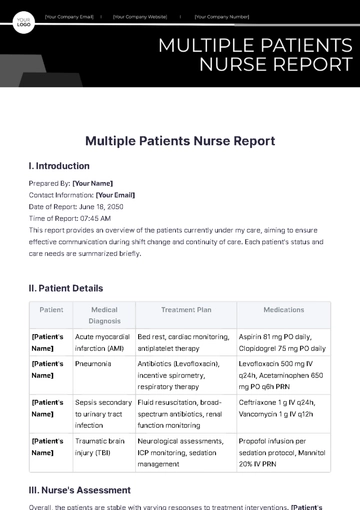
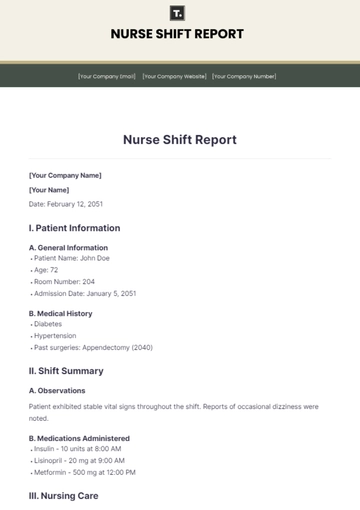
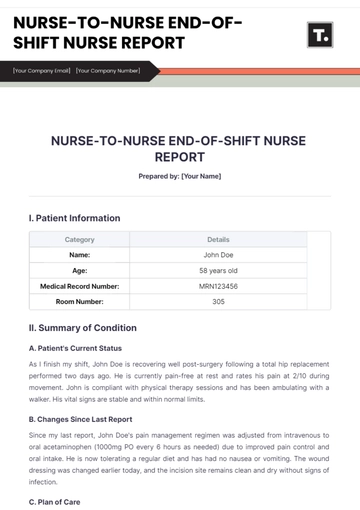
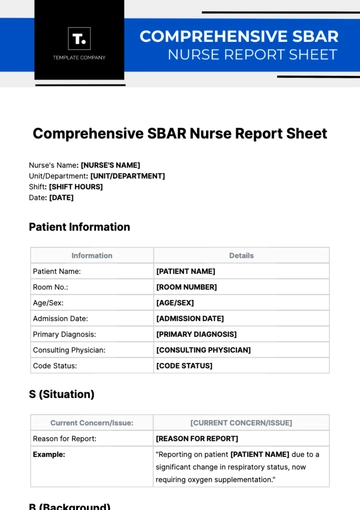
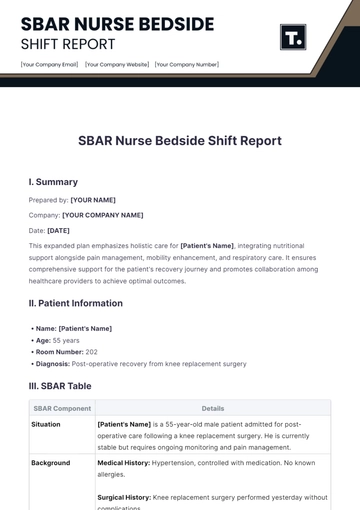
Free Nurse-To-Nurse End of Shift Nurse Report
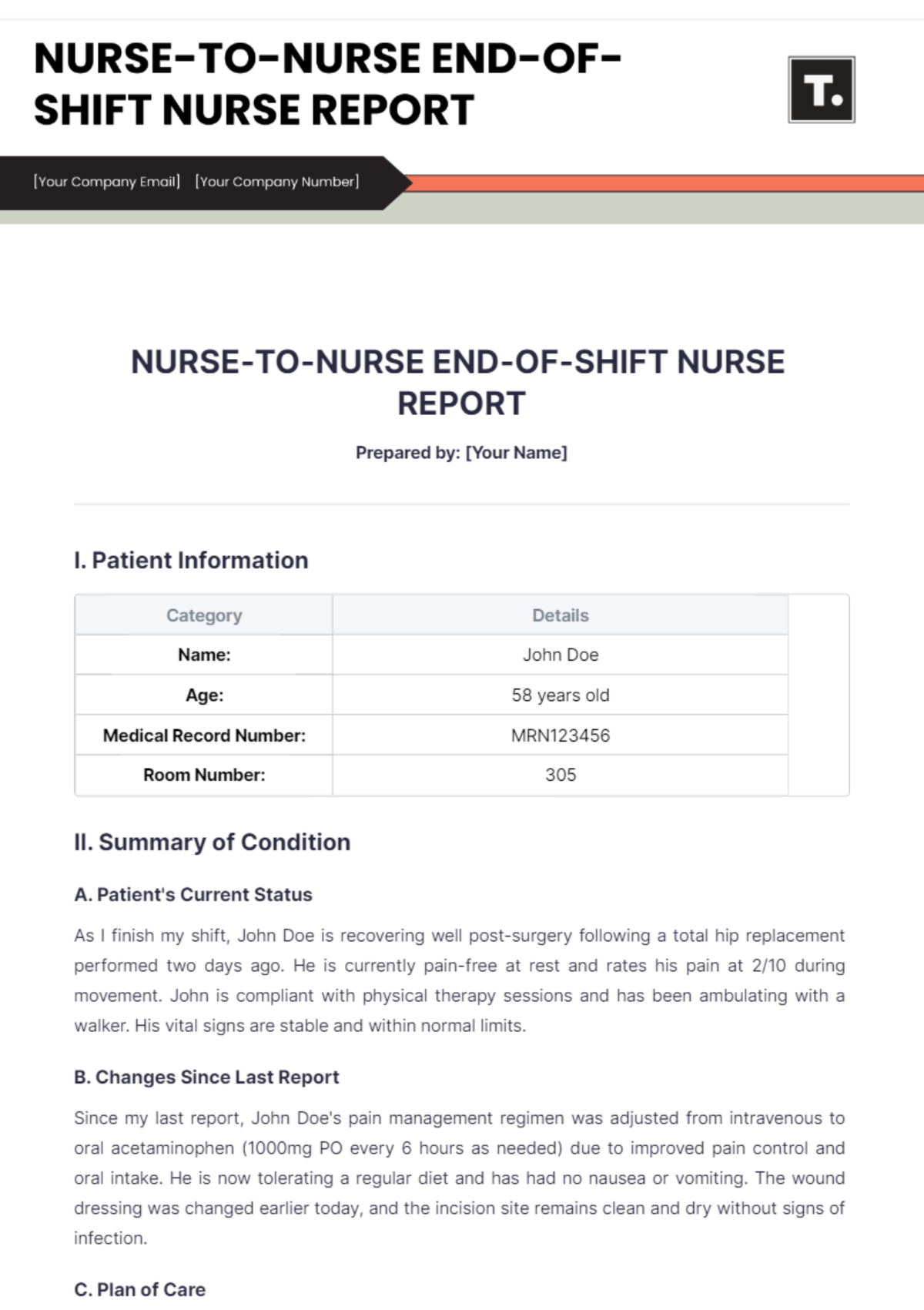
Prepared by: [Your Name]
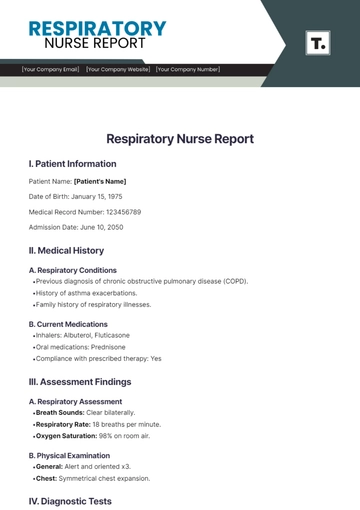
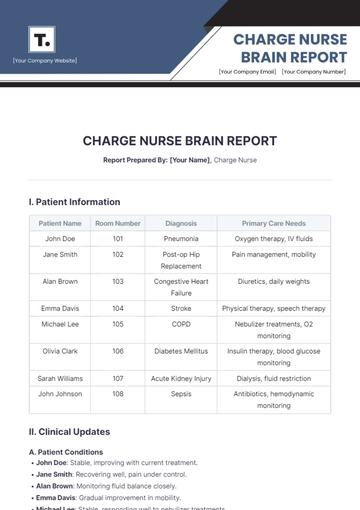
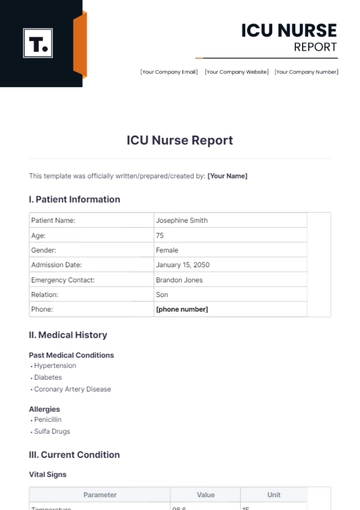
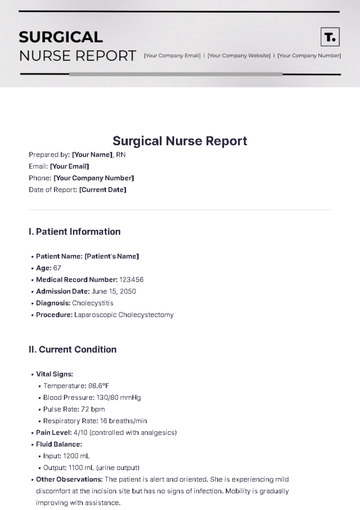
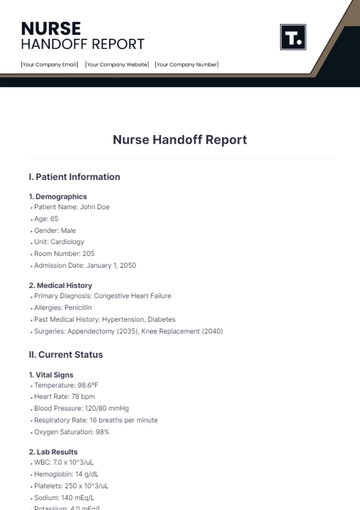
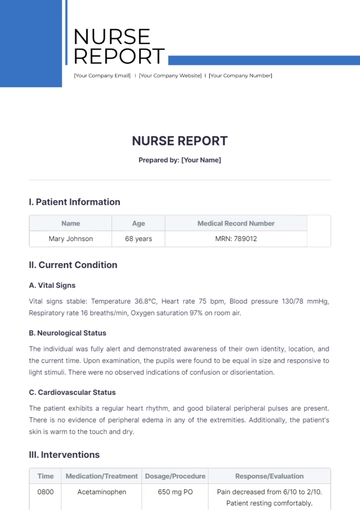
I. Patient Information
Category | Details |
|---|---|
Name: | John Doe |
Age: | 58 years old |
Medical Record Number: | MRN123456 |
Room Number: | 305 |
II. Summary of Condition
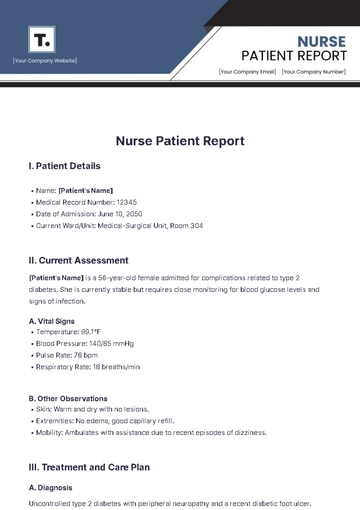
A. Patient's Current Status
As I finish my shift, John Doe is recovering well post-surgery following a total hip replacement performed two days ago. He is currently pain-free at rest and rates his pain at 2/10 during movement. John is compliant with physical therapy sessions and has been ambulating with a walker. His vital signs are stable and within normal limits.
B. Changes Since Last Report
Since my last report, John Doe's pain management regimen was adjusted from intravenous to oral acetaminophen (1000mg PO every 6 hours as needed) due to improved pain control and oral intake. He is now tolerating a regular diet and has had no nausea or vomiting. The wound dressing was changed earlier today, and the incision site remains clean and dry without signs of infection.
C. Plan of Care
The current plan of care includes continued monitoring of pain levels, assistance with mobility as needed, ensuring adequate hydration, and educating the patient on deep breathing exercises to prevent respiratory complications post-surgery. Anticipate discharge planning for tomorrow pending physician assessment.
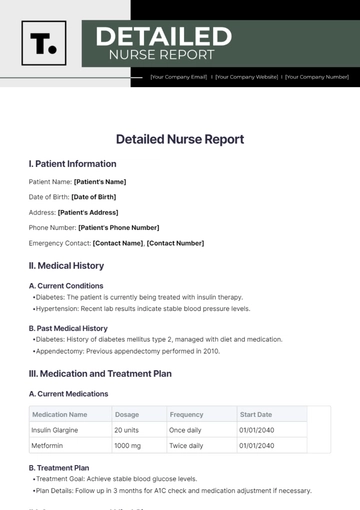
III. Medical History
Condition/Issue | Details |
|---|---|
Past Medical History: | Hypertension, Type 2 Diabetes, Osteoarthritis |
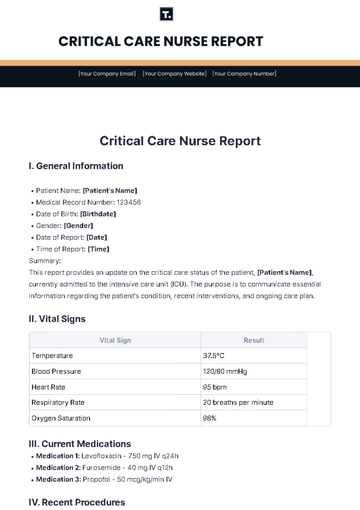
IV. Current Medications
Medication Name | Dosage | Administration Time |
|---|---|---|
Acetaminophen | 1000mg PO | Every 6 hours as needed |
Metformin | 1000mg PO | Daily with breakfast |
Losartan | 50mg PO | Daily |
V. Allergies
Allergen | Reaction |
|---|---|
Penicillin | Rash |
Aspirin | None |
Sulfa Drugs | None |
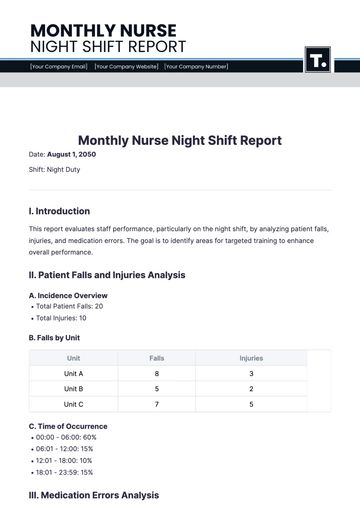
VI. Vital Signs
Vital Sign | Measurement |
|---|---|
Blood Pressure: | 130/80 mmHg |
Heart Rate: | 78 bpm |
Respiratory Rate: | 16 breaths/min |
Temperature: | 98.6°F |
VII. Recent Assessments
Assessment Type | Findings |
|---|---|
Neurological: | Oriented x3, no deficits |
Cardiovascular: | Regular rhythm, no murmurs |
Respiratory: | Clear breath sounds bilaterally |
VIII. Ongoing Treatments
The Treatment/Procedure | Details |
|---|---|
Physical Therapy | Exercises for mobility; patient ambulates with a walker as tolerated |
Wound Care | Incision site clean and dry; dressing changed every 12 hours or as needed |
Patient Education | Deep breathing exercises to prevent atelectasis; review of post-discharge instructions |
IX. Special Instructions
Instruction | Details |
|---|---|
Fall Risk Precautions | Keep the bed in a low position; assist with ambulation; educate the patient on the use of a walker |
Dietary Restrictions | Regular diet; encourage hydration; avoid high-sodium foods to prevent fluid retention |
Discharge Planning | Scheduled for discharge tomorrow pending physician assessment; review discharge instructions with patient and family |
X. Concerns/Issues
A. Patient's Response to Treatment
John Doe has responded well to pain management and physical therapy interventions. Continued encouragement of mobility and deep breathing exercises are recommended to prevent complications.
B. Potential Complications
Monitor for signs of infection at the surgical site, including increased redness, swelling, or drainage. Report any changes promptly to the physician.
C. Recommendations
Coordinate with physical therapy for ongoing rehabilitation exercises. Ensure patient and family understand post-discharge care instructions, including medication management and follow-up appointments.
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
Introducing the Nurse-To-Nurse End of Shift Nurse Report Template from Template.net. This customizable and editable template streamlines shift handovers, ensuring accuracy and efficiency. Easily editable in our Ai Editor Tool, this template caters to your specific needs, making it an indispensable resource for healthcare professionals. Simplify your workflow with Template.net today!
You may also like
- Sales Report
- Daily Report
- Project Report
- Business Report
- Weekly Report
- Incident Report
- Annual Report
- Report Layout
- Report Design
- Progress Report
- Marketing Report
- Company Report
- Monthly Report
- Audit Report
- Status Report
- School Report
- Reports Hr
- Management Report
- Project Status Report
- Handover Report
- Health And Safety Report
- Restaurant Report
- Construction Report
- Research Report
- Evaluation Report
- Investigation Report
- Employee Report
- Advertising Report
- Weekly Status Report
- Project Management Report
- Finance Report
- Service Report
- Technical Report
- Meeting Report
- Quarterly Report
- Inspection Report
- Medical Report
- Test Report
- Summary Report
- Inventory Report
- Valuation Report
- Operations Report
- Payroll Report
- Training Report
- Job Report
- Case Report
- Performance Report
- Board Report
- Internal Audit Report
- Student Report
- Monthly Management Report
- Small Business Report
- Accident Report
- Call Center Report
- Activity Report
- IT and Software Report
- Internship Report
- Visit Report
- Product Report
- Book Report
- Property Report
- Recruitment Report
- University Report
- Event Report
- SEO Report
- Conference Report
- Narrative Report
- Nursing Home Report
- Preschool Report
- Call Report
- Customer Report
- Employee Incident Report
- Accomplishment Report
- Social Media Report
- Work From Home Report
- Security Report
- Damage Report
- Quality Report
- Internal Report
- Nurse Report
- Real Estate Report
- Hotel Report
- Equipment Report
- Credit Report
- Field Report
- Non Profit Report
- Maintenance Report
- News Report
- Survey Report
- Executive Report
- Law Firm Report
- Advertising Agency Report
- Interior Design Report
- Travel Agency Report
- Stock Report
- Salon Report
- Bug Report
- Workplace Report
- Action Report
- Investor Report
- Cleaning Services Report
- Consulting Report
- Freelancer Report
- Site Visit Report
- Trip Report
- Classroom Observation Report
- Vehicle Report
- Final Report
- Software Report