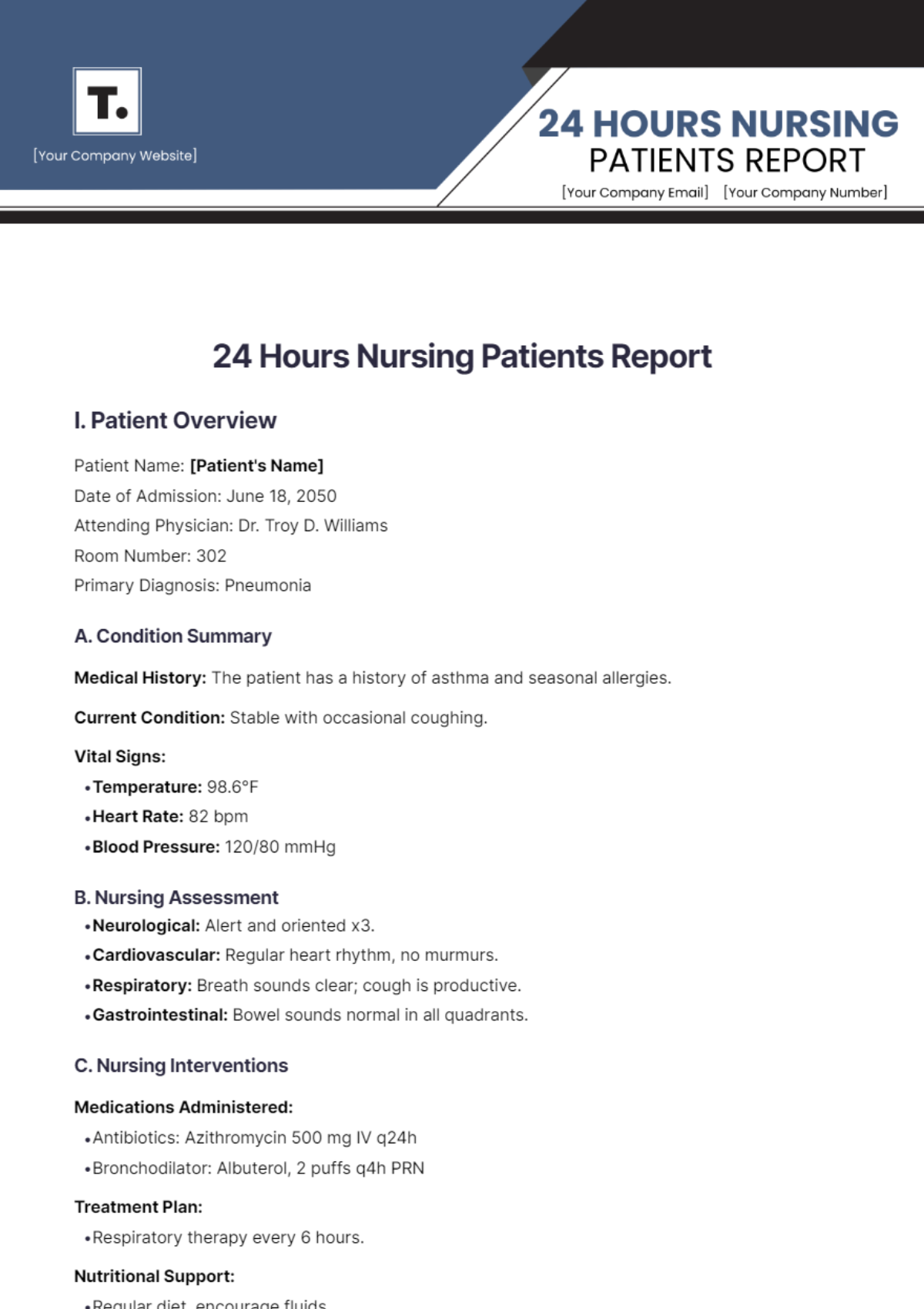
24 Hours Nursing Patients Report
I. Patient Overview
Patient Name: [Patient's Name]
Date of Admission: June 18, 2050
Attending Physician: Dr. Troy D. Williams
Room Number: 302
Primary Diagnosis: Pneumonia
A. Condition Summary
Medical History: The patient has a history of asthma and seasonal allergies.
Current Condition: Stable with occasional coughing.
Vital Signs:
Temperature: 98.6°F
Heart Rate: 82 bpm
Blood Pressure: 120/80 mmHg
B. Nursing Assessment
Neurological: Alert and oriented x3.
Cardiovascular: Regular heart rhythm, no murmurs.
Respiratory: Breath sounds clear; cough is productive.
Gastrointestinal: Bowel sounds normal in all quadrants.
C. Nursing Interventions
Medications Administered:
Antibiotics: Azithromycin 500 mg IV q24h
Bronchodilator: Albuterol, 2 puffs q4h PRN
Treatment Plan:
Respiratory therapy every 6 hours.
Nutritional Support:
Regular diet, encourage fluids.
II. Nursing Care Plan
A. Nursing Diagnosis
Priority: Impaired Gas Exchange related to pneumonia.
Goals:
Improve oxygenation levels.
Decrease cough frequency.
B. Interventions
Physical Care:
Encourage deep breathing exercises.
Monitor oxygen saturation levels.
Emotional Support:
Provide reassurance and explain procedures.
Patient Education:
Educate on the importance of respiratory hygiene.
III. Progress Notes
A. Shift Change Report
Evening Shift (June 18, 2050):
The patient was admitted with a productive cough and started on antibiotics.
Night Shift (June 18–19, 2050):
Their vital signs were stable, and they responded well to bronchodilator therapy.
B. 24-Hour Summary
General Observations:
The patient remains stable, and coughing is less frequent.
Nursing Response:
Increased respiratory assessments due to productive cough.
IV. Discharge Planning
A. Discharge Goals
Expected Discharge Date: June 20, 2050
Recommendations:
Continue taking antibiotics at home for the prescribed duration.
Follow-up with primary care physician in one week.
B. Follow-Up Care
Post-Discharge Care Plan:
Provide discharge instructions and medication schedule.