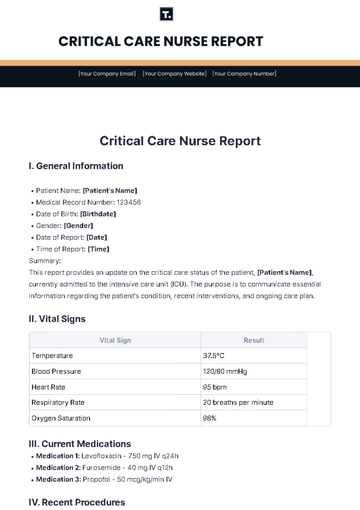
Free Critical Care Nurse Report
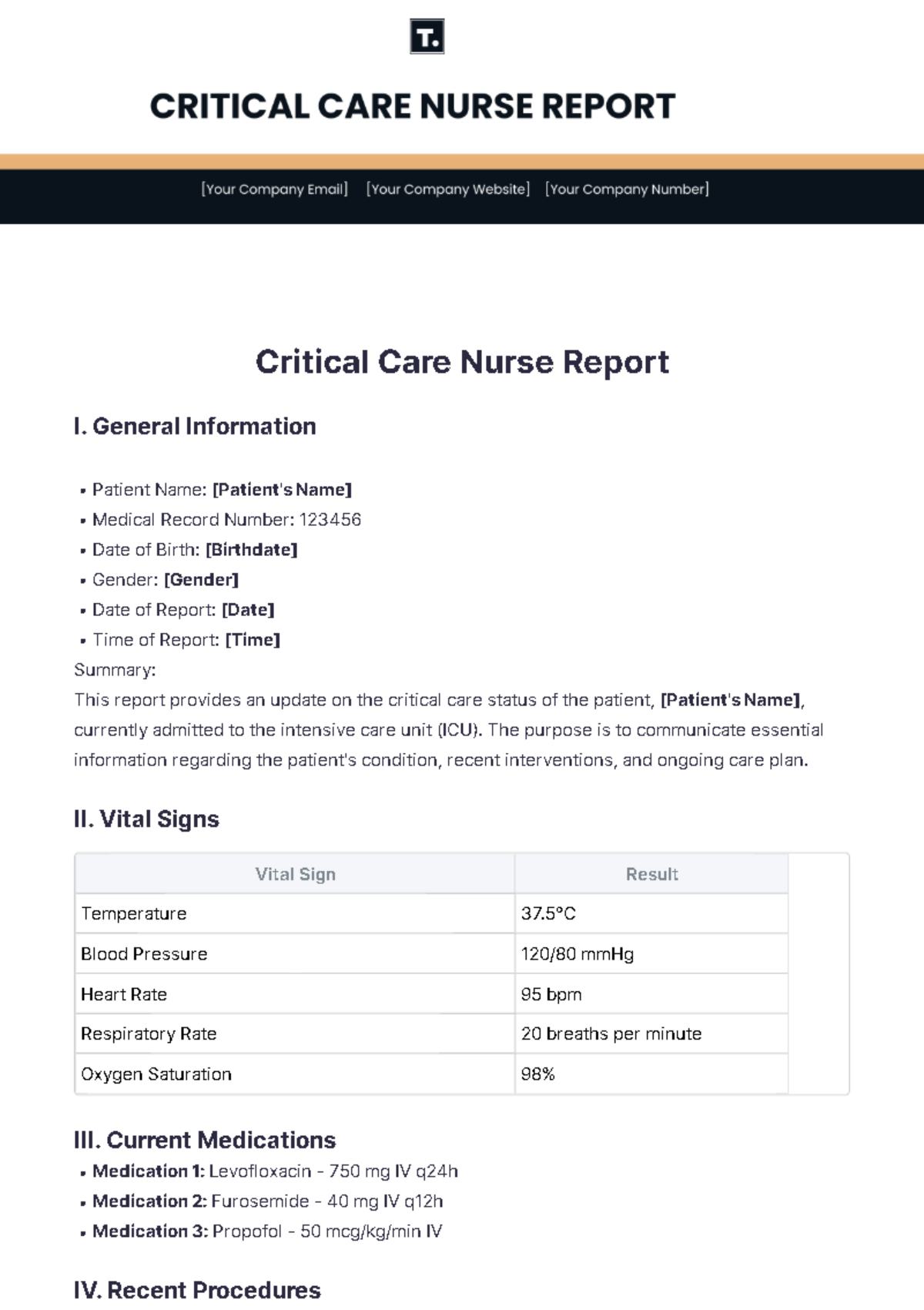
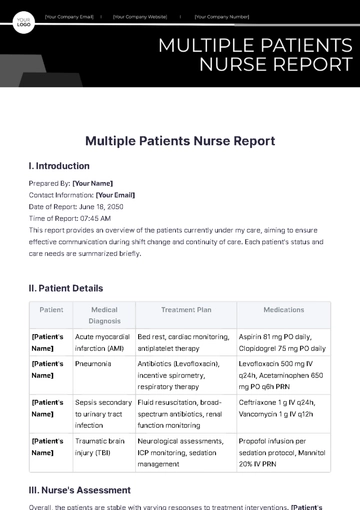
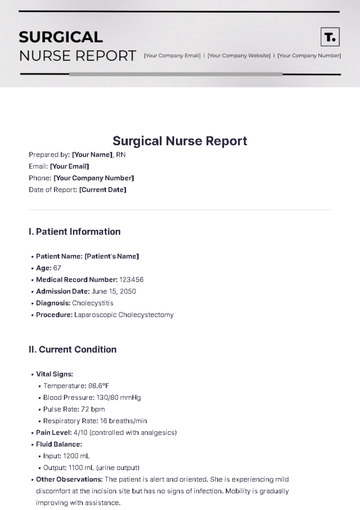
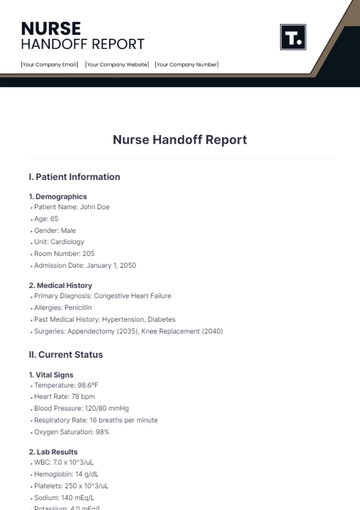
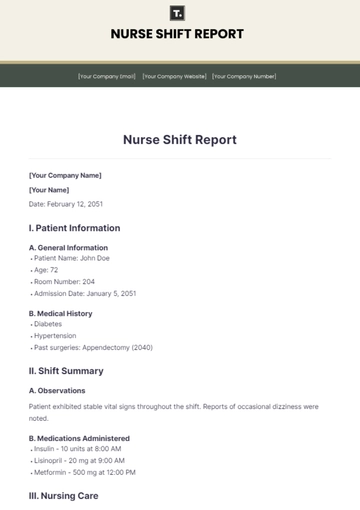
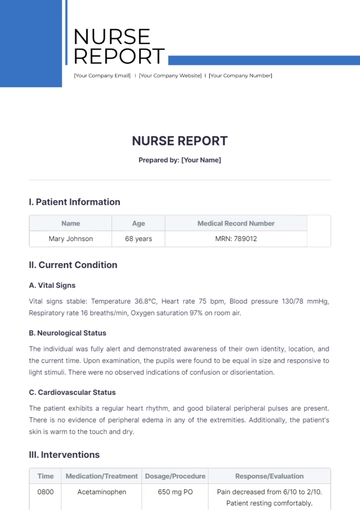
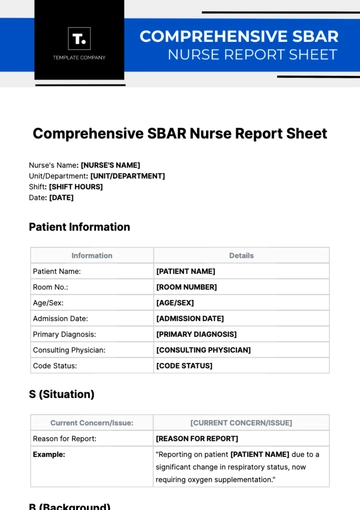
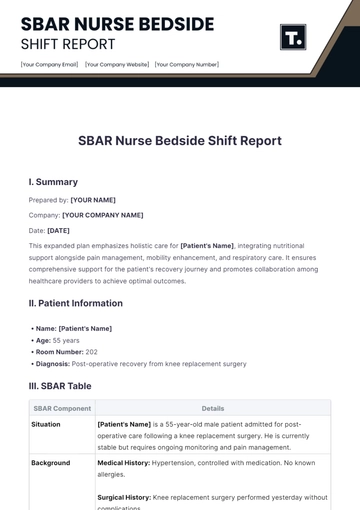
I. General Information
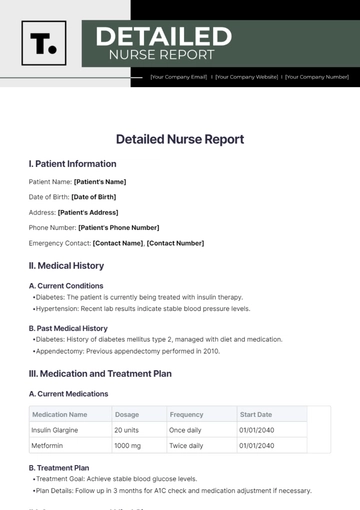
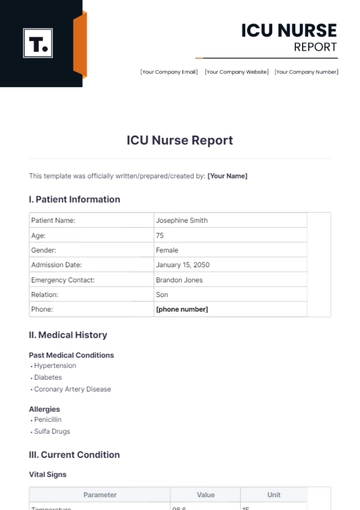
Patient Name: [Patient's Name]
Medical Record Number: 123456
Date of Birth: [Birthdate]
Gender: [Gender]
Date of Report: [Date]
Time of Report: [Time]
Summary:
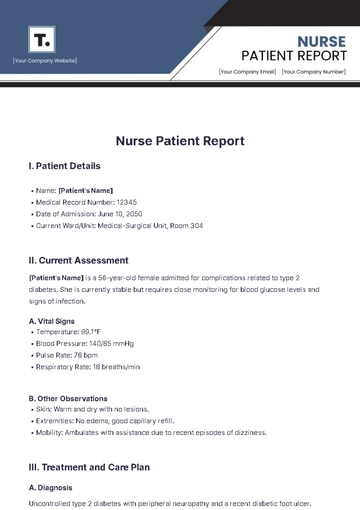
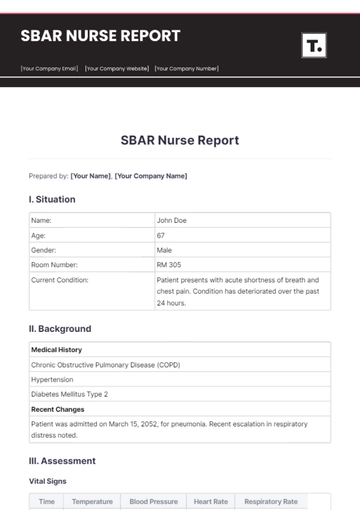
This report provides an update on the critical care status of the patient, [Patient's Name], currently admitted to the intensive care unit (ICU). The purpose is to communicate essential information regarding the patient's condition, recent interventions, and ongoing care plan.
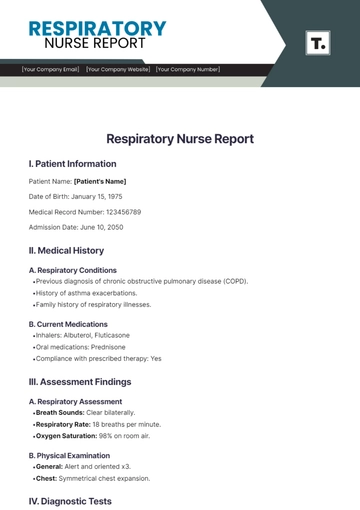
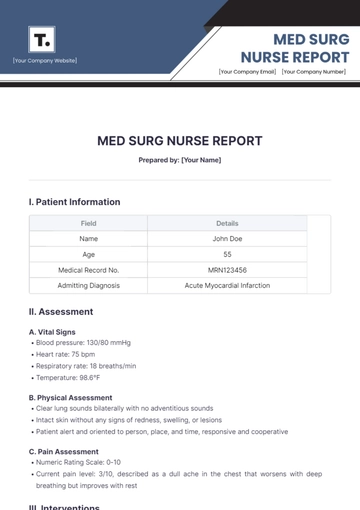
II. Vital Signs
Vital Sign | Result |
|---|---|
Temperature | 37.5°C |
Blood Pressure | 120/80 mmHg |
Heart Rate | 95 bpm |
Respiratory Rate | 20 breaths per minute |
Oxygen Saturation | 98% |
III. Current Medications
Medication 1: Levofloxacin - 750 mg IV q24h
Medication 2: Furosemide - 40 mg IV q12h
Medication 3: Propofol - 50 mcg/kg/min IV
IV. Recent Procedures
Central line placement: Successful, no complications.
Arterial blood gas (ABG) analysis: pH 7.35, PaO2 90 mmHg, PaCO2 40 mmHg.
V. Assessment
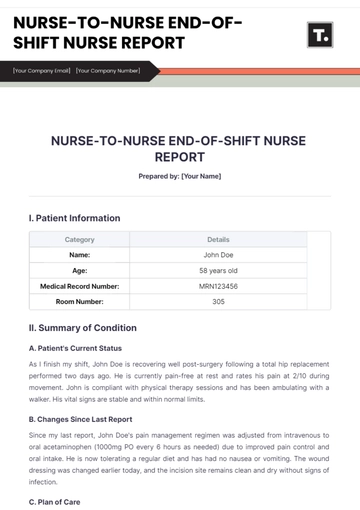
[Patient's Name] remains stable following admission to the ICU with improved respiratory function noted post-intubation. Vital signs indicate maintained hemodynamic stability, with blood pressure within normal limits and heart rate steady. Laboratory results reveal a reduction in inflammatory markers, suggesting a positive response to initial antibiotic therapy.
However, ongoing support with vasopressors is necessary to maintain adequate perfusion. Neurological assessments show responsiveness to stimuli, indicating preserved neurological function at this time. The patient's condition warrants continued close monitoring, particularly for any signs of sepsis recurrence or respiratory compromise.
VI. Plan
Immediate Plan | Short-term Plan | Long-term Plan |
|---|---|---|
|
|
|
VII. Nurse's Notes
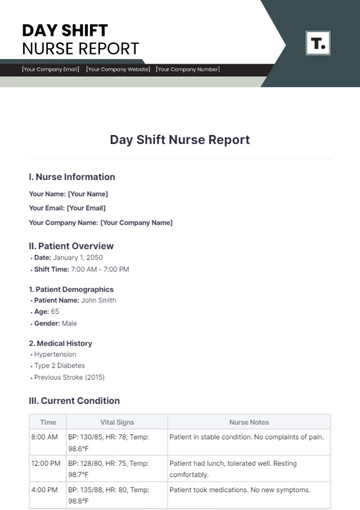
Response to Treatment: [Patient's Name] has shown improved oxygenation and stable ventilator settings post-intubation.
Family Communication: Regular updates provided to the family, who remain supportive and engaged in care discussions.
Comfort Measures: Nursing interventions focused on maintaining patient comfort throughout the shift.
Sedation Management: Ensured adequate sedation levels to optimize patient comfort and respiratory support.
Infection Control: Strict adherence to infection control protocols to minimize risk of secondary infections.
Prepared by:

[Your Name], RN
Nurse On Duty
- 100% Customizable, free editor
- Access 1 Million+ Templates, photo’s & graphics
- Download or share as a template
- Click and replace photos, graphics, text, backgrounds
- Resize, crop, AI write & more
- Access advanced editor
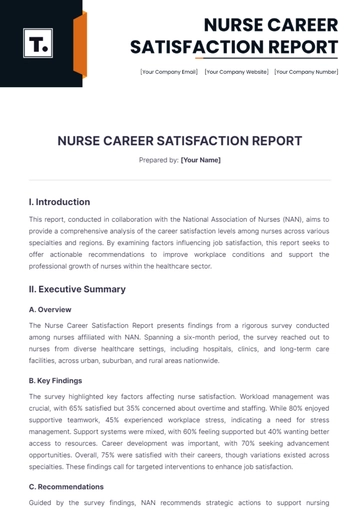
Enhace patient care with the Critical Care Nurse Report Template by Template.net. Designed for critical care environments, this customizable and downloadable template ensures accurate and detailed patient reporting. It’s printable and editable in our AI Editor Tool, providing nurses with an efficient way to document patient conditions and care activities. Ensure your critical care documentation is precise and professional.
You may also like
- Sales Report
- Daily Report
- Project Report
- Business Report
- Weekly Report
- Incident Report
- Annual Report
- Report Layout
- Report Design
- Progress Report
- Marketing Report
- Company Report
- Monthly Report
- Audit Report
- Status Report
- School Report
- Reports Hr
- Management Report
- Project Status Report
- Handover Report
- Health And Safety Report
- Restaurant Report
- Construction Report
- Research Report
- Evaluation Report
- Investigation Report
- Employee Report
- Advertising Report
- Weekly Status Report
- Project Management Report
- Finance Report
- Service Report
- Technical Report
- Meeting Report
- Quarterly Report
- Inspection Report
- Medical Report
- Test Report
- Summary Report
- Inventory Report
- Valuation Report
- Operations Report
- Payroll Report
- Training Report
- Job Report
- Case Report
- Performance Report
- Board Report
- Internal Audit Report
- Student Report
- Monthly Management Report
- Small Business Report
- Accident Report
- Call Center Report
- Activity Report
- IT and Software Report
- Internship Report
- Visit Report
- Product Report
- Book Report
- Property Report
- Recruitment Report
- University Report
- Event Report
- SEO Report
- Conference Report
- Narrative Report
- Nursing Home Report
- Preschool Report
- Call Report
- Customer Report
- Employee Incident Report
- Accomplishment Report
- Social Media Report
- Work From Home Report
- Security Report
- Damage Report
- Quality Report
- Internal Report
- Nurse Report
- Real Estate Report
- Hotel Report
- Equipment Report
- Credit Report
- Field Report
- Non Profit Report
- Maintenance Report
- News Report
- Survey Report
- Executive Report
- Law Firm Report
- Advertising Agency Report
- Interior Design Report
- Travel Agency Report
- Stock Report
- Salon Report
- Bug Report
- Workplace Report
- Action Report
- Investor Report
- Cleaning Services Report
- Consulting Report
- Freelancer Report
- Site Visit Report
- Trip Report
- Classroom Observation Report
- Vehicle Report
- Final Report
- Software Report