CLINICAL SUMMARY SHEET LAYOUT
Introduction
A Clinical Summary Sheet is a vital document in patient care, providing an overarching view of a patient's medical history, current condition, treatments, and test results. This document assists healthcare professionals in making informed decisions, enhancing the quality and efficiency of care.
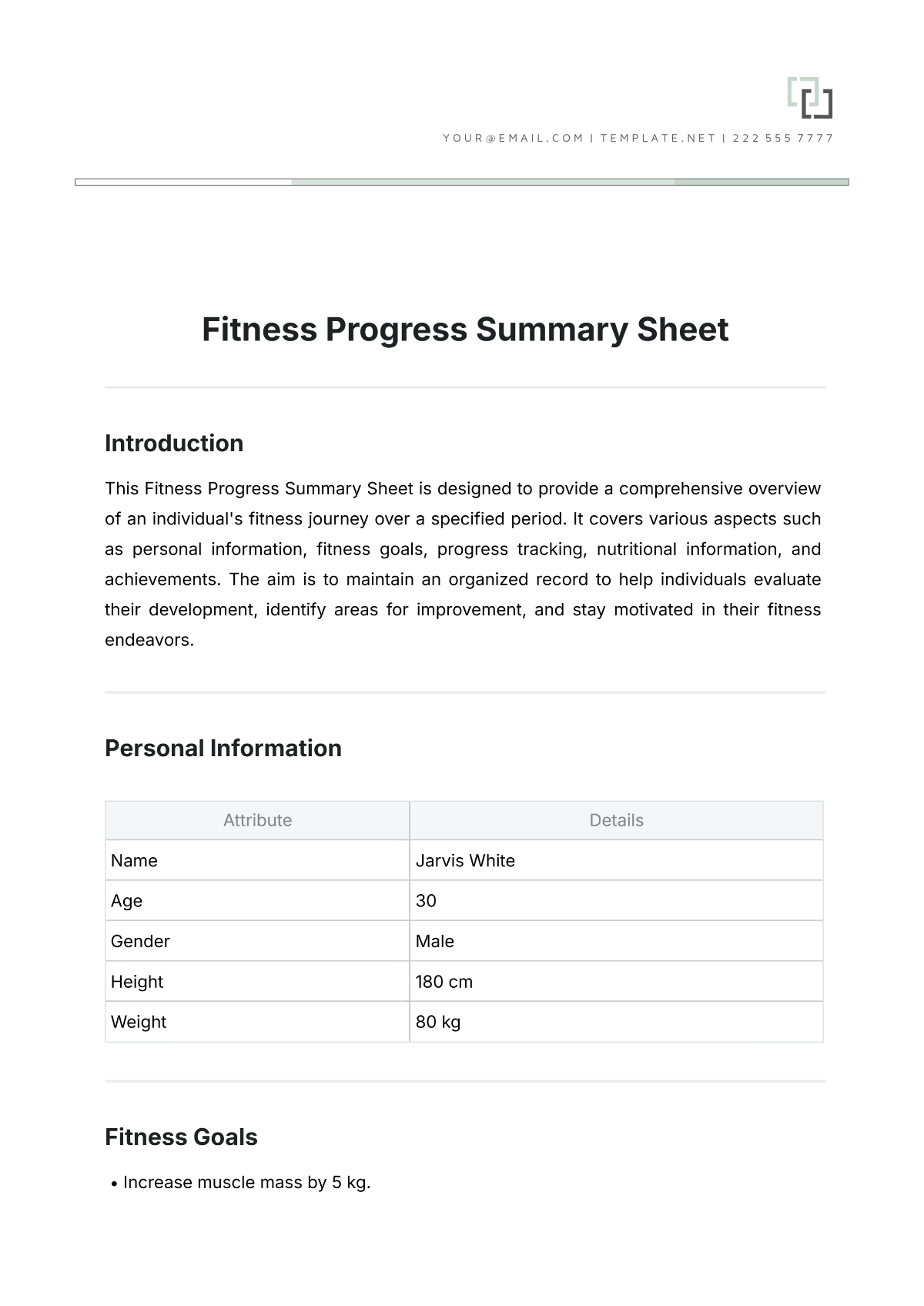
Basic Patient Information
The basic patient information section contains essential details that identify and provide context about the patient.
Patient Name: [Insert Patient Name]
Date of Birth: [Insert Date of Birth]
Gender: [Insert Gender]
Patient ID: [Insert Patient ID]
Contact Information: [Insert Contact Information]
Medical History
This section records the patient's past medical history, chronic conditions, surgeries, and any recurring treatments. It is crucial for understanding the patient's background and potential health risks.
Chronic Conditions: [Insert Chronic Conditions]
Previous Surgeries: [Insert Previous Surgeries]
Known Allergies: [Insert Known Allergies]
Family History of Diseases: [Insert Family History of Diseases]
Previous Hospitalizations: [Insert Previous Hospitalizations]
Current Medications
The current medications section lists all medications that the patient is presently taking, including dosage and frequency. This ensures that care providers are aware of ongoing treatments to avoid contraindications and facilitate effective medication planning.
Drug Name: [Insert Drug Name]
Dosage: [Insert Dosage]
Frequency: [Insert Frequency]
Prescribing Physician: [Insert Prescribing Physician]
Vital Signs
Monitoring patient vital signs is critical for assessing current health status. This section provides the latest records and trends of the patient's key physiological parameters.
Vital Sign | Reading | Date Recorded |
|---|---|---|
Temperature | [Insert Reading] | [Insert Date Recorded] |
Blood Pressure | [Insert Reading] | [Insert Date Recorded] |
Heart Rate | [Insert Reading] | [Insert Date Recorded] |
Respiratory Rate | [Insert Reading] | [Insert Date Recorded] |
Laboratory Results
The laboratory results section is essential for reviewing diagnostic data, identifying abnormalities, and tracking progress over time. Each entry includes test name, results, date, and reference ranges.
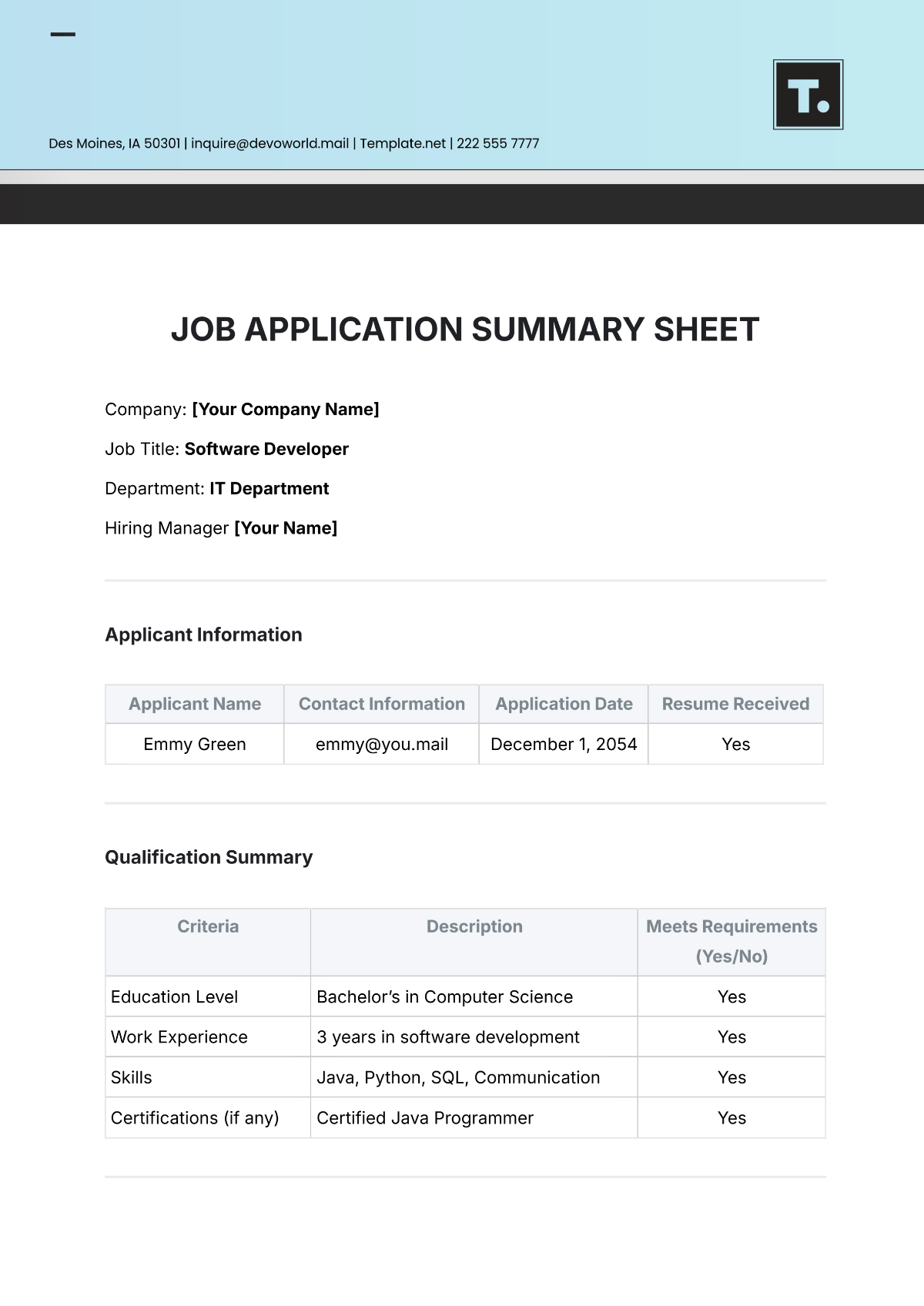
Test Name | Result | Date | Reference Range |
|---|---|---|---|
Complete Blood Count (CBC) | [Insert Result] | [Insert Date] | White cells: 4,500 to 11,000 cells/mcL |
Basic Metabolic Panel (BMP) | [Insert Result] | [Insert Date] | Sodium: 135-145 mmol/L |
Lipid Panel | [Insert Result] | [Insert Date] | Cholesterol: Lower than 200 mg/dL |
Imaging Results
This section includes findings from imaging studies that provide insights into the patient's internal structures. Reports should detail the type of imaging, findings, and any relevant observations made by specialists.
Imaging Type (e.g., X-ray, MRI, CT Scan): [Insert Imaging Type]
Date of Imaging: [Insert Date of Imaging]
Findings and Observations: [Insert Findings and Observations]
Radiologist’s Comments: [Insert Radiologist’s Comments]
Treatment Plan
The treatment plan outlines current and proposed treatments, including medications, therapies, and lifestyle recommendations. This section emphasizes personalized patient care and follow-up plans.
Medications and Adjustments: [Insert Medications and Adjustments]
Physical or Occupational Therapy: [Insert Therapy]
Surgical Interventions: [Insert Interventions]
Dietary Modifications: [Insert Dietary Modifications]
Follow-up Appointments: [Insert Follow-up Appointments]
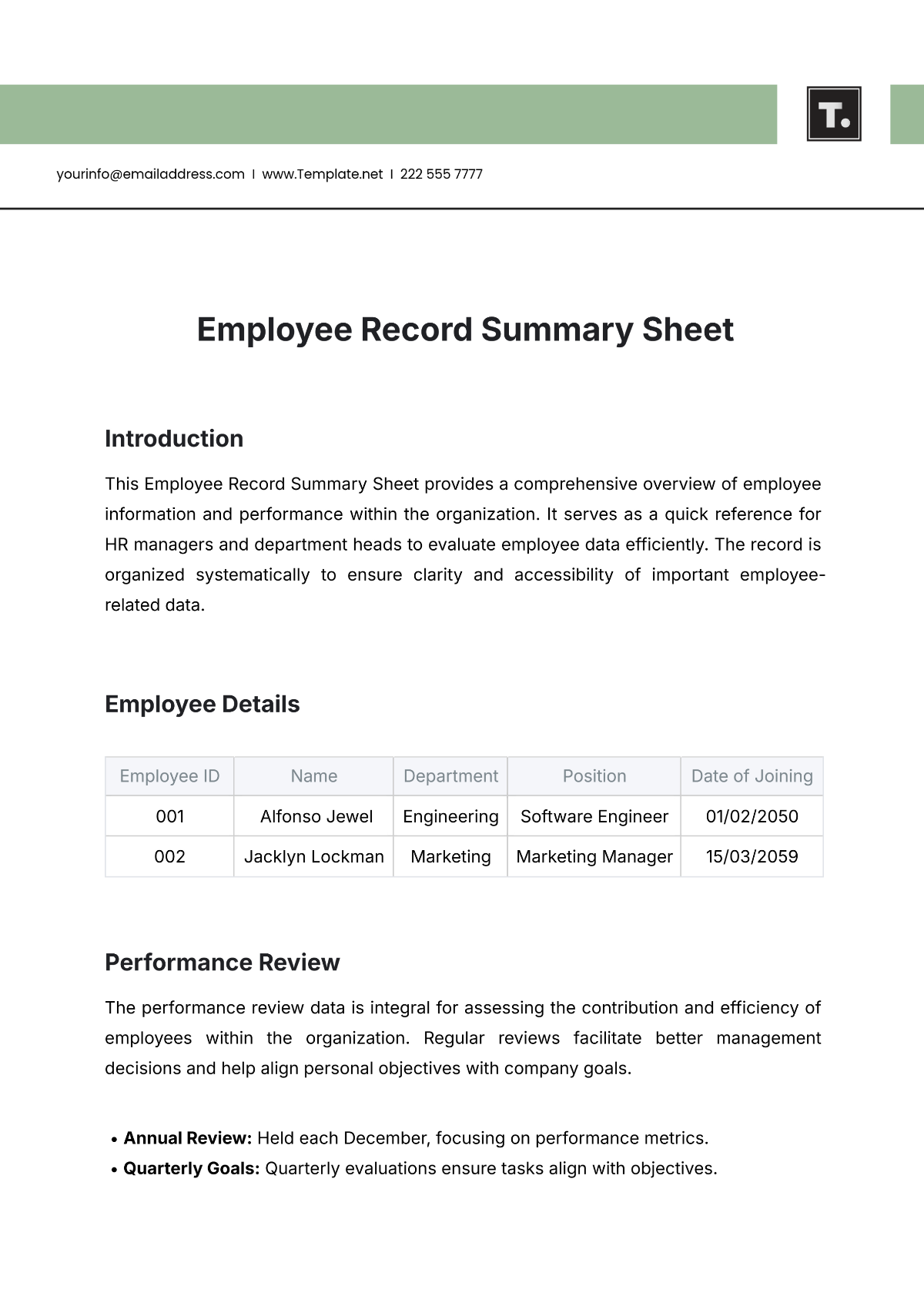
Provider's Notes
The provider's notes give a narrative of the patient's care journey, summarizing changes in condition, responses to treatments, and any consultative input from other healthcare specialists.
Summary of Care Provided: [Insert Summary of Care Provided]
Observations and Assessments: [Insert Observations and Assessments]
Interdisciplinary Consultations: [Insert Consultations]
Conclusion
The Clinical Summary Sheet plays a critical role in streamlining patient information for efficient review by healthcare providers. By regularly updating and maintaining detailed records, providers can ensure continuity and quality of care, ultimately improving patient outcomes.